The dengue virus forms a distinct complex under the genus flaviviruses based on antigenic and biological characteristics. There are four dengue virus serotypes which are designated as DENV-1, DENV-2, DENV-3, and DENV-4. A recent study in 2017 (until February 2018) in Dhaka, described DENV-2 as the dominant type, but also detected some DENV-1 and DENV-3. In the present study, despite a small sample size, DENV-3 accounted for 46% of the samples in September and October 2018, Infection with anyone of these serotypes confers lifelong immunity to that virus serotype. Although all four serotypes are antigenically similar yet they elicit cross protection for only few months. Secondary infection with dengue serotype 2 or multiple infection with different serotypes enhance chances of occurring more severe form of diseases.
1.2 Epidemiology
exp date isn't null, but text field is
The epidemiology of dengue exhibits a complex relationship among host (man and mosquito), agent (virus) and the environment. These relationships determine the level of endemicity in an area. The transmission of dengue remains low due to extremes of temperature with low relative humidity. Temperatures in the range of 25°C ± 5°C, relative humidity around 80% and innumerable small water collections result high transmission.
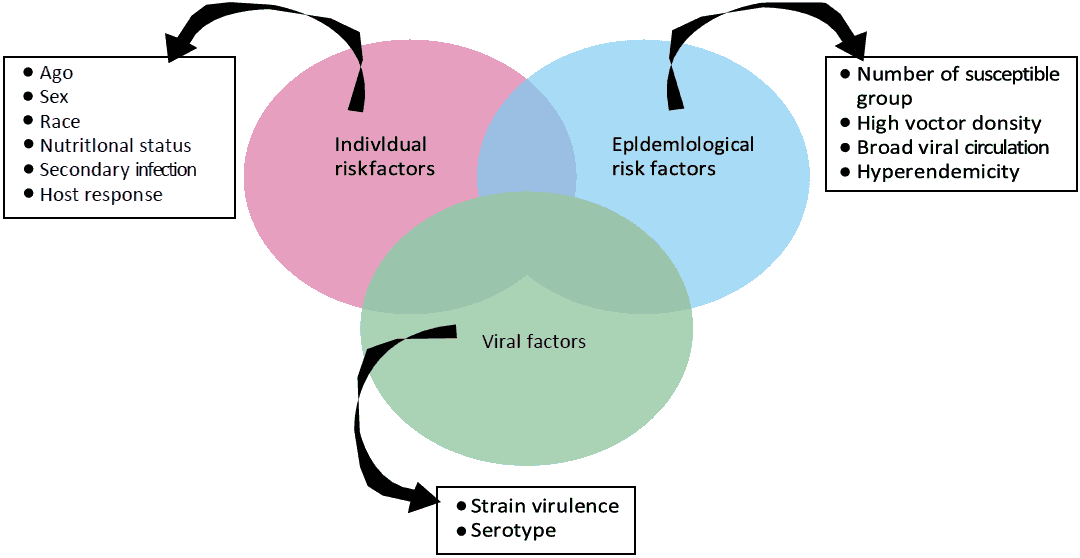
Figure 1 Dengue Epidemiological Triad
Aedes aegypti is the primary vector and Aedes albopictus is secondary vector for dengue in Bangladesh. Aedes aegypti is highly domesticated and strongly anthropophilic. It needs more than one bite to complete one blood meal and needs more than one blood meal to complete one gonotropic cycle.
These habits result in the generation of multiple cases and clustering of dengue cases in the cities Aedes aegypti breeds almost entirely in domestic man-made water receptacles found in and around households, water storage containers, water reservoirs, overhead tanks, desert coolers, unused tires, coconut shells, disposable cups, unused grinding stones, industrial and domestic junk, construction sites, etc.
Results of Aedes Survey in the year 2019 conducted by Communicable Disease Control (CDC) unit of Directorate General of Health Services (DGHS) shows percentages of positive breeding sources during pre-monsoon, monsoon and post-monsoon showed high positivity rates in drinking water storages (plastic drums, buckets and water tanks) at pre & post monsoon indicating safe water scarcity.
Larval positivity rates reduced may be due to enhanced awareness among the urban inhabitant other breeding source.
A. albopictus is an aggressive feeder and can take the amount of blood they need for each gonotropic cycle in one bite. They usually are distributed in the peripheral areas of urban cities. It prefers natural larval habitats which include tree holes, latex collecting cups in rubber plantations, leaf axils, bamboo stumps, coconut shells, etc.
The female usually becomes infected with the dengue virus when it takes a blood meal from a person during the acute febrile (viremia) phase of dengue illness. After an extrinsic incubation period of 8 to 10 days, the mosquito becomes infected. The virus is transmitted when the infected female mosquito bites and injects its saliva into the wound of the person bitten. The cycle of dengue continues by this process. Dengue begins abruptly after an intrinsic incubation period of 4 to 7 days (range 3–14 days). There is also evidence of vertical transmission of dengue virus from infected female mosquitoes to the next generation.
Before 1970, only nine countries had experienced severe dengue epidemics. Today, the disease is endemic in more than 100 countries throughout the globe. The actual numbers of dengue cases are under reported and many cases are misclassified. World Health Organization estimate indicates that 390 million dengue infections occur every year (95% credible interval 284–528 million), of which 96 million (67–136 million) manifest clinically (with any severity of disease). Another (2012) study, of the prevalence of dengue, estimates that 3.9 billion people in 128 countries are at risk of infection with dengue viruses.
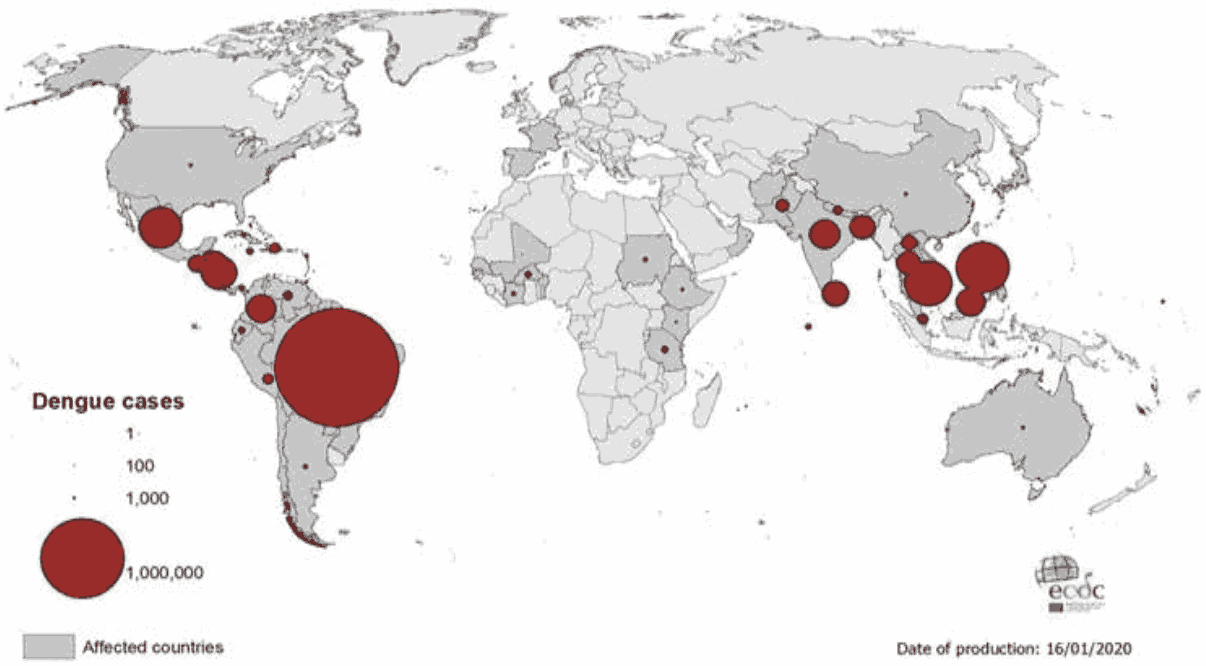
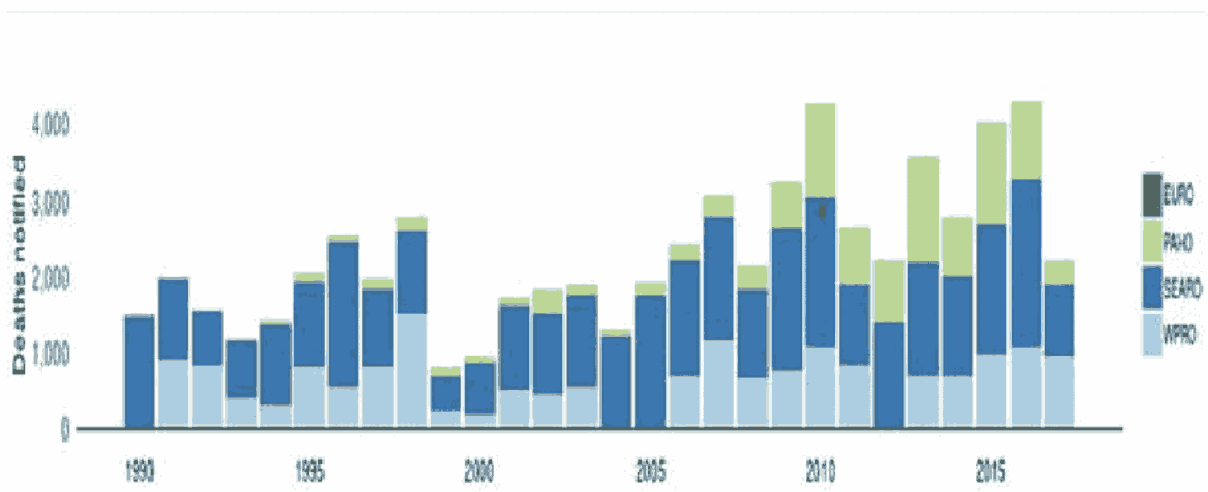
Figure 2 Dengue Cases among WHO Regions
The first epidemic of dengue hemorrhagic fever occurred in mid-2000 when 5,551 dengue infections were reported from Dhaka, Chittagong, and Khulna cities, occurring mainly among adults. Among the reported cases- 4,385 (62.4%) cases were Dengue Fever (DF) and 1,186 (37.6%) cases were Dengue Hemorrhagic Fever (DHF). The Case-Fatality Rate (CFR) was 1.7%, with 93 reported deaths. Aedes aegypti was identified as the main vector responsible for the epidemic, also Aedes albopictus was identified as a potential vector in Chittagong. According to WHO, the worst outbreak occurred in 2002, with 6,232 cases and 58 deaths.
In the year 2019 dengue case burden was the worst with 101354 cases and 179 deaths and proliferation of cases spread were not limited to major cities but to most of the districts of Bangladesh. Since 2000-2004, the average of number of annual cases was 3,626; which is quite high in comparison to the last 5 years (2015-2019) average of 24,614. However, the average number of deaths was same ranges from 41-42.
The prevalent serotypes of dengue virus are DENV-1, DENV-2, DENV-3 and DENV-4 with the highest number of reported cases attributed to DENV-3. A similar situation can be seen in other countries, such as India and Sri Lanka, where DENV3 has been reported most of the time in DF/DHF-related illnesses.
Over the last 10-15 years, dengue fever and dengue hemorrhagic fever have become the leading causes of hospitalization and death among both children and adults in South-East Asian regions. The dengue cases are reported based upon information collected from the Control Room at the DGHS. The source of information is mainly the public sector, private clinics and some selected urban NGOs. Moreover, the information sources at present are based in Dhaka city. Information from other parts of the country is still insufficient. So, it is very difficult to come to a definitive conclusion regarding the program perspective.
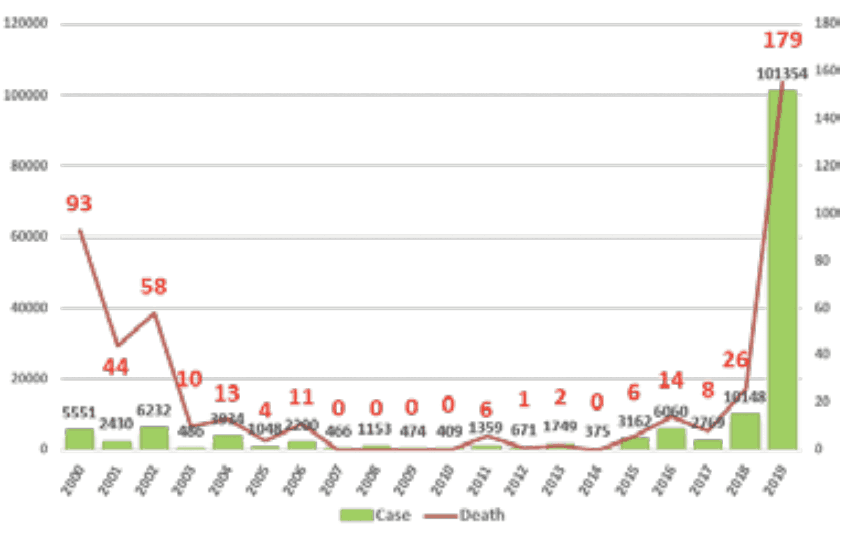
Figure 3 - Number of Dengue Cases and Death in Bangladesh (2000-2019)
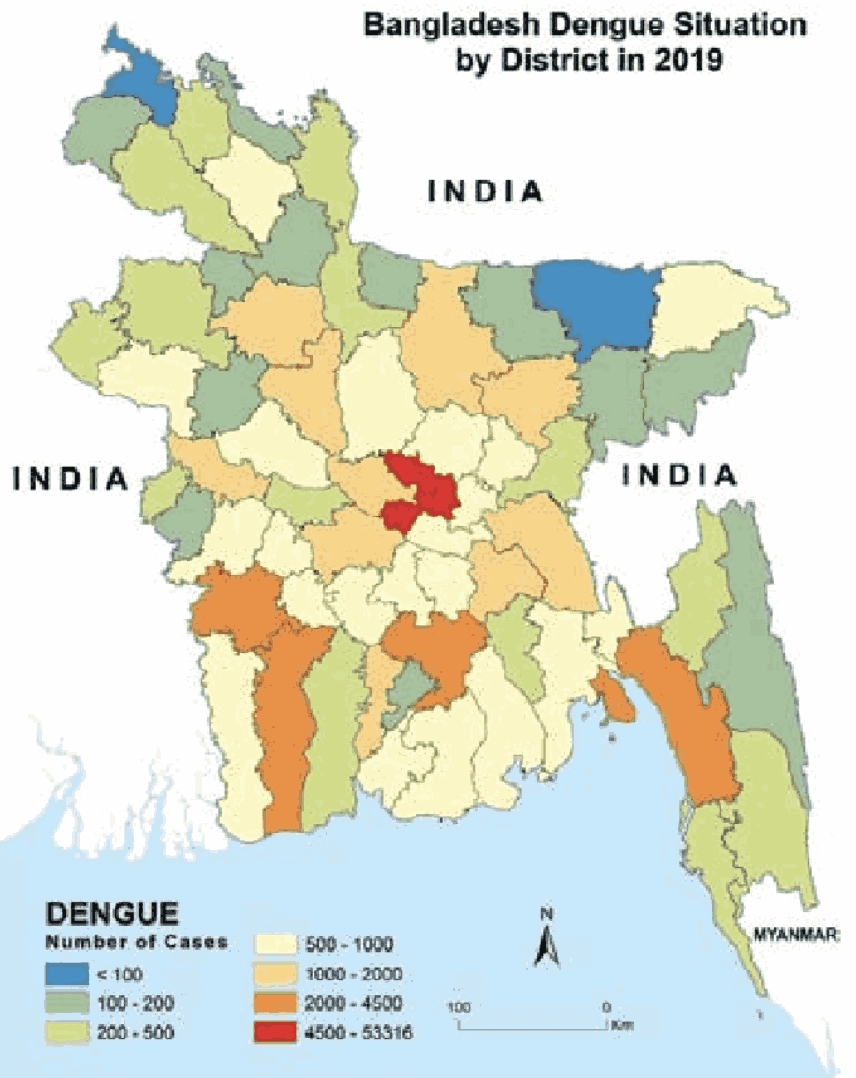
Figure 4 - Dengue Prevalence in Bangladesh
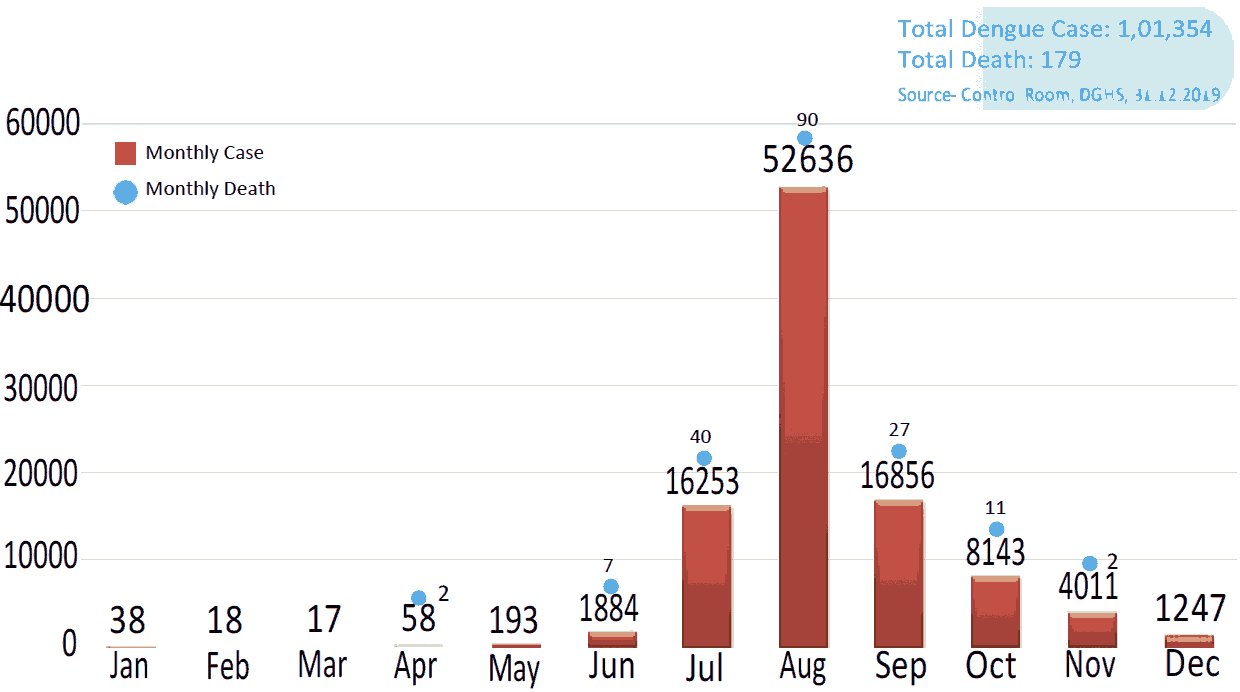
Figure 5 - Graphical presentation of dengue cases in Bangladesh 2019
