Majority of dengue virus infections are asymptomatic. However, age appears to influence the prevalence of symptomatic disease. The majority of infections in children under age 15 years are asymptomatic or minimally symptomatic.
2.2 Clinical Manifestation of Dengue Infection
exp date isn't null, but text field is
Many patients infected with dengue virus remain asymptomatic. Others, after an incubation period of 4-7 (range 3-14) days, develop a febrile illness the manifestations of which are similar and overlapping in nature grouped into ‘Dengue Syndromes’ which encompass the following:
- Undifferentiated fever
- DF
- DHF
- Expanded Dengue Syndrome (rare)
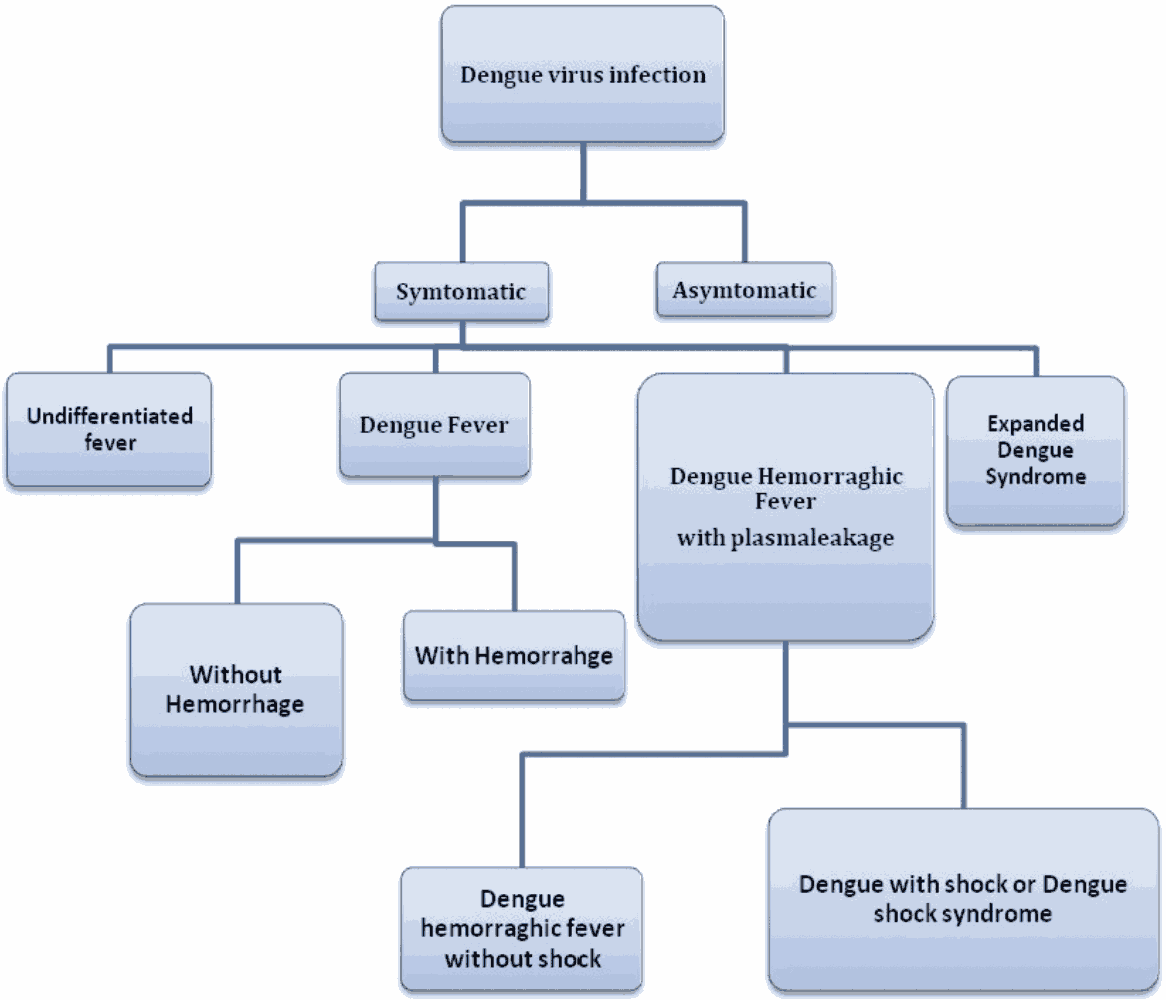
Figure 8 - Clinical Manifestation of Dengue
Undifferentiated fever
Those who have been infected with dengue virus, especially for the first time (i.e. primary dengue infection), may develop a simple fever indistinguishable from other viral infections. Maculopapular rashes may accompany the fever or may appear during defervescence. Upper respiratory and gastrointestinal symptoms are common.
Dengue fever
Typically, the onset of DF is sudden with a sharp rise in temperature and is frequently associated with a flushed face and headache. Occasionally, chills accompany the sudden rise in temperature. The following features are usually observed:
- Retro-orbital pain on eye movement or pressure on eye
- Photophobia
- Backache and pain in the muscles and joints/bones.
- The other common symptoms include anorexia and altered taste sensation, constipation, colicky pain and abdominal tenderness.
It is noteworthy that these symptoms and signs of DF vary markedly in frequency and severity.
Fever:
The body temperature is usually between 39°C and 40°C (102°F to 104°F) and the fever may be biphasic, lasting 2-7 days in the majority of cases.
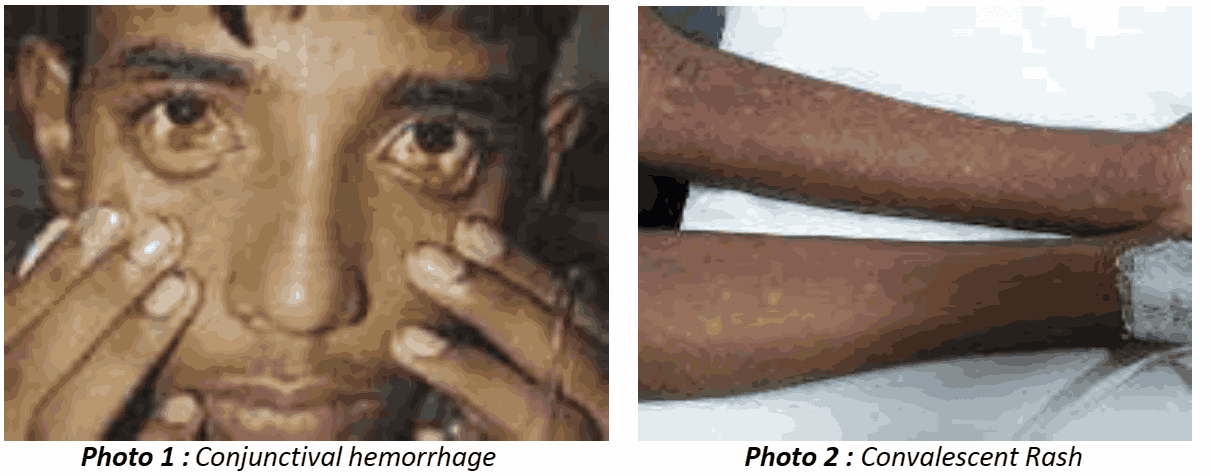
Rash:
- First 2 to 3 days-Diffuse flushing or fleeting eruptions may be seen on the face, neck and chest
- Third and fourth day-a conspicuous rash that may be maculopapular or rubelliform
- Afebrile period or defervescence - Petechiae surrounding scattered pale, round areas of normal skin may appear over the dorsum of the feet, on the legs, and on the hands and arms. Skin itching maybe observed.
Hemorrhagic manifestations:
In DF with unusual hemorrhage, Petechiae may be present. Other bleeding such as massive epistaxis, menorrhagia and gastrointestinal bleeding rarely occur in DF, complicated with thrombocytopenia. Tourniquet test will be positive in this case.
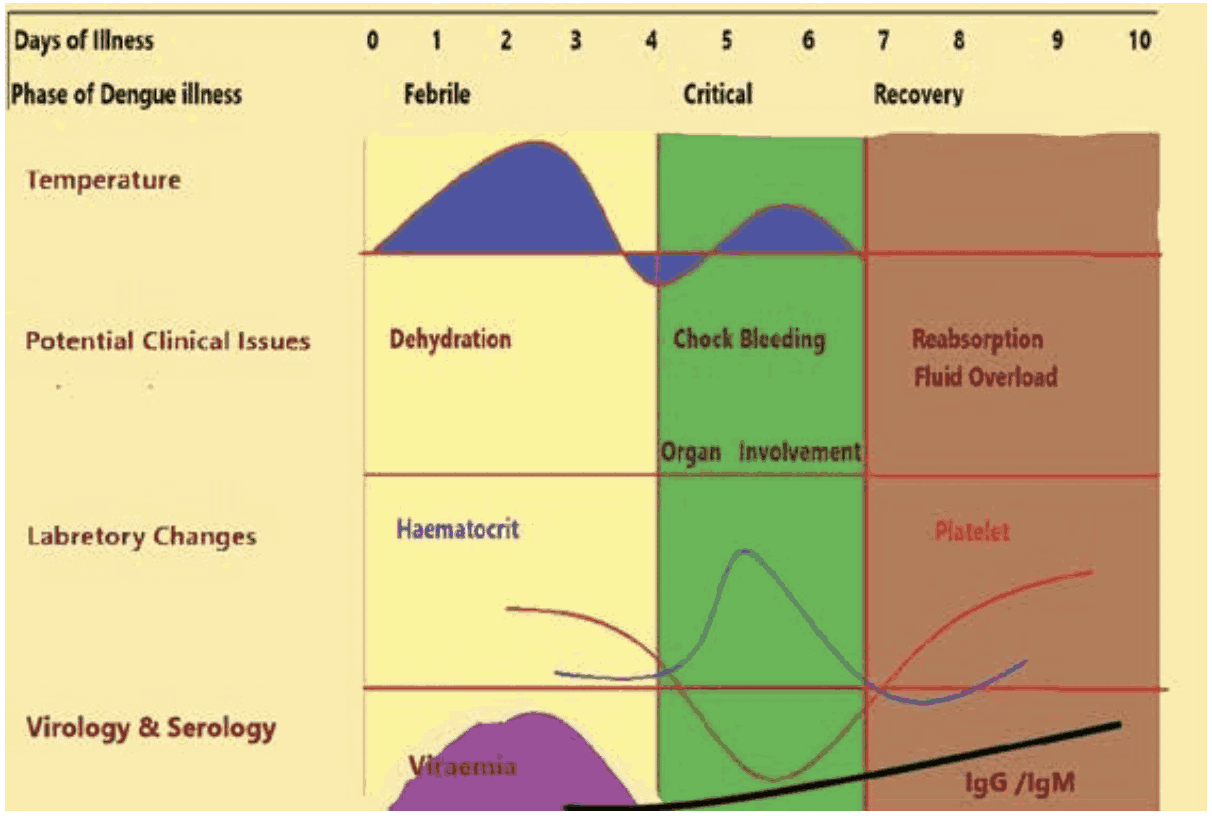
Figure 9 - Clinical Course of Dengue Fever
Dengue Hemorrhagic fever
DHF is characterized by the acute onset of high fever and is associated with signs and symptoms similar to DF in the early febrile phase. Critical phase with plasma leakage is the hallmark of DHF which occurs soon after the end of the febrile phase. There is a tendency to develop hypovolemic shock (dengue shock syndrome) due to plasma leakage.
Hemorrhagic Manifestation:
The clinical course of illness passes through the following three phases:
- Febrile phase
- Critical phase
- Convalescent phase
Febrile Phase
The onset of dengue fever is usually with sudden rise in temperature which may be biphasic, lasting 2-7 days and commonly associated with headache, flushing and rash. There may be pain in retro-orbital area, muscles, joint or bone. Rash may be maculopapular or rubelliform and usually appear after 3 or 4 days of fever and commonly seen in face, neck and other part of the body which generally fades away in the later part of the febrile phase. Localized cluster of petechiae may appear over upper and lower limbs.
Critical Phase
DF/DHF patients usually go to critical phase after 3 to 4 days of onset of fever. During this critical phase plasma leakage and high haemoconcentration are documented and patients may develop hypotension. Abnormal haemostasis and leakage of plasma leads to shock, bleeding, accumulation of fluid in pleural and abdominal cavity. High morbidity and mortality in DHF/DSS are commonly associated with various organ involvements and metabolic derangement. The period of plasma leakage usually persists for 36-48 hrs. Commonly in DHF, platelet count is less than 100000 per/cumm of blood.
Convalescent Phase
During the recovery phase the extracellular fluid which was lost due to capillary leakage returns to the circulatory system and signs and symptoms improve. This phase usually after 6-7 days of fever and last for 2-3 days. Longer convalescence may be expected in some of the patients with severe shock, organ involvement and other complications which may require specific treatment. Patient may develop pulmonary oedema due to fluid overload if the fluid replacement is not optimized carefully.
Evidence of Plasma leakage
- Haematocrit (HcT) - With the leakage of plasma there will increase in HcT. A 20% rise of HcT from the baseline is indicative of significant plasma leakage.
- Plasma leakage is due to increased capillary permeability.
- Plasma leakage in DHF is selective and transient and usually lasts for 24-48 hours.
- Ascites and pleural effusion may develop.
Therefore, early detection of critical period (onset of plasma leakage) and appropriate fluid management is of paramount importance. These patients may develop overt or concealed bleeding during the course of illness.
Other evidence of plasma leakage is:
- non-fasting serum cholesterol (<100 mg/dl).
- The degree and the rate of plasma leakage in DHF can vary.
- Severe leakage may develop shock, which may be complicated with organ impairment, metabolic acidosis and disseminated intravascular coagulation (DIC).
Tourniquet Test (TT)
This is a very important clinical test for detecting covert hemorrhage. The tourniquet test is performed by inflating a blood pressure cuff applied usually to the forearm to a point mid-way between the systolic and diastolic pressures for five minutes. After deflating wait for return of normal skin hue and then count the number of petechie. A test is considered positive when 10 or more petechiae per 1 inch² are observed in the exposed part below the cuff. In DHF, the test usually gives a definite positive result when there is ≥ 20 petechiae per 1 inch² with a sensitivity of more than 90%. Sometimes in lieu of petechiae linear steaks of echymosis may be seen in the cuff applied area. The test may be negative or mildly positive only during the phase of profound shock.
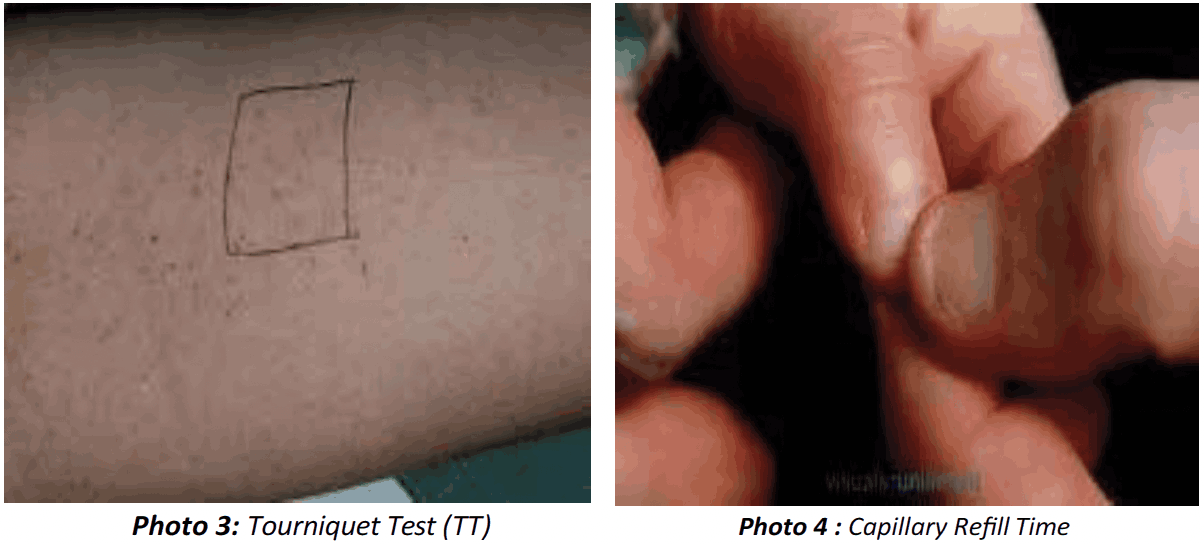
Capillary Refill Time
This is a clinical examination for volume status of the body. It can be measured by pressing the nail of the thumb of left hand in right handed person or vice versa till blanching then suddenly release the pressure. The time taken for flushing is the capillary refill time and if it is more than 3 sec, there is gross hypovolumia.
Dengue Shock Syndrome
Significant loss of plasma leads to hypovolemic shock. Even in these shock cases, prior to intravenous fluid therapy, pleural effusion and ascites may not be detected clinically. Radiographic and ultrasound evidence of plasma leakage precedes clinical detection. A right lateral decubitus chest radiograph to detect pleural effusion and gall bladder wall oedema is associated with plasma leakage and may precede the clinical detection.
Dengue Shock Syndrome is a prevention of Dengue Syndromes when there are criteria of DHF plus signs of circulatory failure, manifested by:
- Rapid and weak pulse
- Narrow pulse pressure (≤ to 20 mm Hg)
- Hypotension for age
- Cold clammy skin
- Restlessness
- Undetectable pulse and blood pressure
Expanded Dengue Syndrome/Isolated Organopathy (unusual manifestations)
Patients with dengue illness can sometimes develop unusual manifestations such as involvement of liver, kidneys, brain or heart with or without evidence of fluid leakage and therefore do not necessarily fall into the category of DHF. These conditions are very rare and management is symptomatic. Such unusual manifestations may be associated with coinfections and comorbidities. However, these manifestations if seen in DHF patients are mostly a result of prolonged shock leading to organ failure.
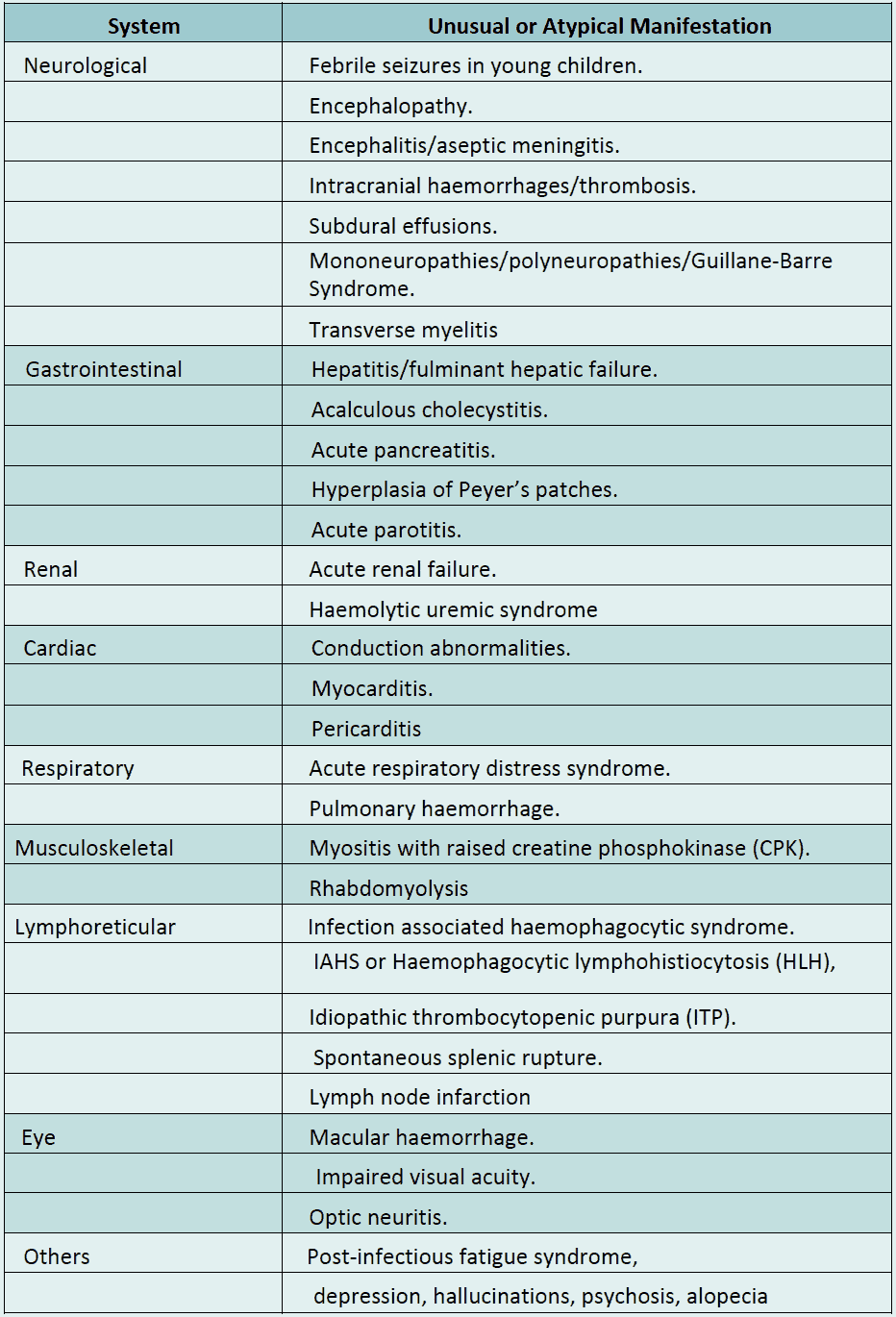
Table 1 : Expended Dengue Syndrome
