4.2 Stepwise Approach of Dengue Case Management
exp date isn't null, but text field is
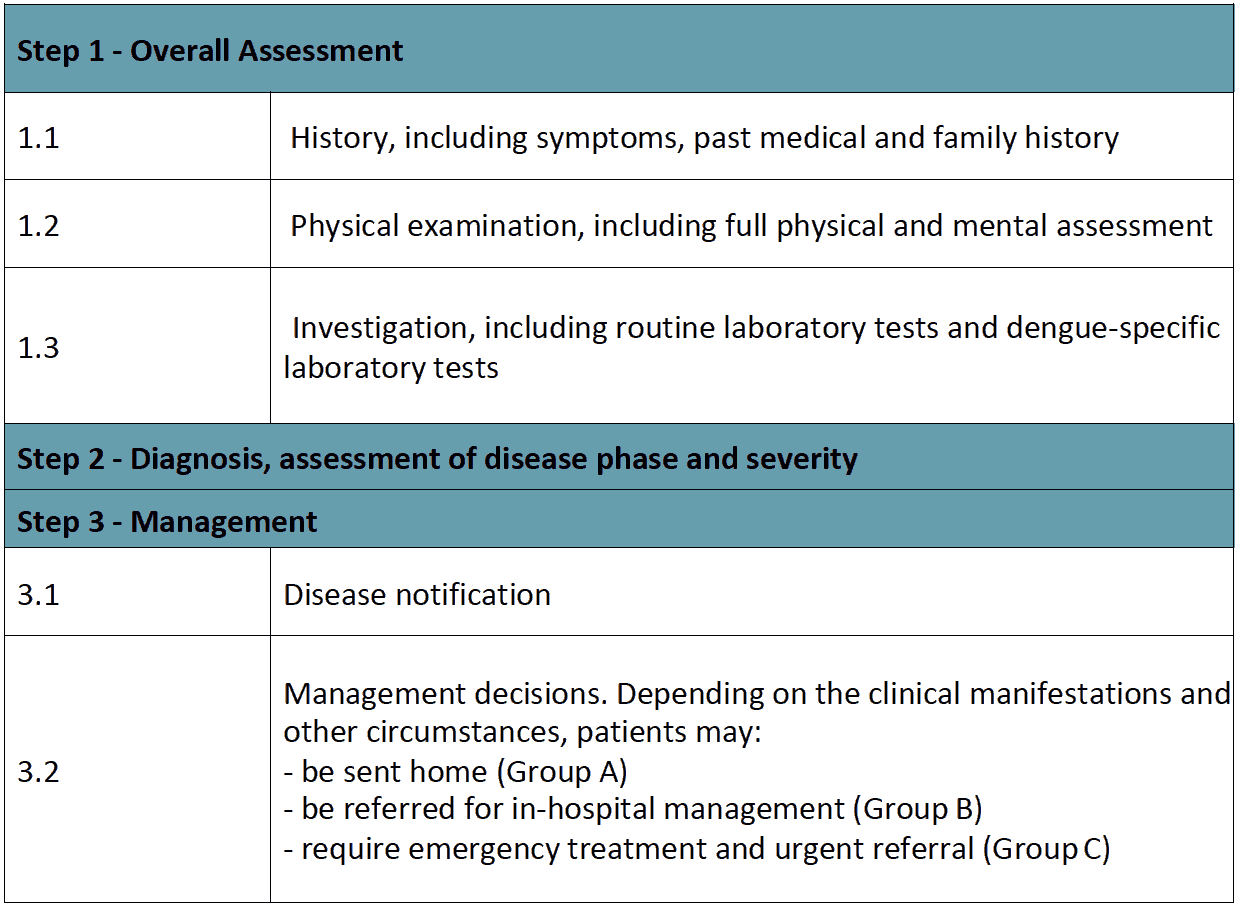
Table 8 - Step Wise Dengue Case Management
Step 1 – Overall assessment
1.1 The history should include:
- Date of onset of fever/illness;
- Quantity of oral fluid intake;
- Diarrhoea;
- Urine output (frequency, volume and time of last voiding);
- Assessment of warning signs;
- Change in mental state/seizure/dizziness;
- Other important relevant history, such as family or neighbourhood dengue, travel to dengue-endemic areas, co-existing conditions (e.g. infancy, pregnancy, obesity, diabetes mellitus, hypertension), jungle trekking and swimming in waterfalls (consider leptospirosis, typhus, malaria), recent unprotected sex or drug abuse (consider acute HIV-seroconversion illness).
1.2 The physical examination should include
- Assessment of mental state;
- Assessment of hydration status;
- Assessment of haemodynamic status;
- Checking for quiet tachypnoea/acidotic breathing/pleural effusion;
- Checking for abdominal tenderness/hepatomegaly/ascites;
- Examination for rash and bleeding manifestations;
- Tourniquet test (repeat if previously negative or if there is no bleeding manifestation).
1.3 The investigation
- A full blood count (CBC) should be done at the first visit (it may be normal); Platelet count and haematocrit repeated daily until the critical phase is over.
- The haematocrit in the early febrile phase could be used as the patient’s own baseline.
- Decreasing white blood cell and platelet counts make the diagnosis of dengue very likely.
- Leukopenia usually precedes the onset of the critical phase and has been associated with severe disease.
- A rapid decrease in platelet count, concomitant with a rising haematocrit compared to the baseline, is suggestive of progress to the plasma leakage/critical phase of the disease.
- These changes are usually preceded by leukopenia (≤ 5000 cells/mm3). In the absence of the patient’s baseline, age-specific population haematocrit levels could be used as a surrogate during the critical phase.
- If facilities for a full blood count are not available or if resources are limited, such as in outbreak settings, a full blood count or microhaematocrit should be done at the first visit to establish the baseline. This should be repeated after the 3rd day of illness and in those with warning signs and risk factors for severe disease.
- Dengue-specific laboratory tests should be performed to confirm the diagnosis. However, it is not necessary for the acute management of patients, except in cases with unusual manifestations.
Additional tests should be considered in patients with co-morbidities and severe disease as indicated. These may include tests of liver function, glucose, serum electrolytes, urea and albumin.
Step 2 - Diagnosis, Assessment of disease phase and severity
Diagnosis, assessment of disease phase and severity on the basis of evaluations of the history, physical examination and/or full blood count and haematocrit.
Clinicians should determine whether the disease is dengue, which phase it is in (febrile, critical or recovery), whether there are warning signs, the hydration and haemodynamic state of the patient, and whether the patient requires admission. For blood pressure assessment follow age specific blood pressure chart (see annexure).
Step 3 - Management
- Disease notification in dengue-endemic countries:
Suspected dengue: acute febrile illness with or without non-specific signs and symptoms.
Probable dengue: an acute febrile illness with serological diagnosis.
Confirmed dengue: An acute febrile illness with positive dengue NS1 antigen or PCR test.
- For the purpose of the management the definition of the cases will be defined as group A, B & C. During the time of reporting both will be incorporate in the reporting system.
- Laboratory confirmation is not necessary before notification, but it should be obtained.
In non-endemic countries, usually only confirmed cases will be notified.
- Management decisions: Depending on the clinical manifestations and other circumstances, patients may-
- either be sent home (Group A);
- be referred for in-hospital management (Group B); or
- require emergency treatment and urgent referral (Group C).
