- Impact on physiology of pregnancy.
- Cardiovascular - tachycardia, lower blood pressure.
- Hematological - lower HcT at 3rd trimester.
- HCO3 (Bicarbonate) level - lower.
The following physiological changes in pregnancy may make the diagnosis and assessment of plasma leakage challenging:
- Elevation of HcT in dengue is marked by hemodilution due to increase in plasma volume especially in the 2nd and 3rd trimester.
- Serial HcT measurement is crucial for disease monitoring in pregnancy.
- The detection of third space fluid accumulation is difficult due to the presence of gravid uterus.
- Baseline blood pressure is often lower and pulse pressure wider.
- Baseline heart rate may be higher.
Impact of dengue on pregnancy and delivery.
- Early Abortion (3%-13%).
- Embryopathy specially neural tube defect.
- Antepartum haemorrhage (APH) due to retro placental hemorrhage or abruptio placenta.
- Preterm birth (3%-33%).
- Low-birth weight (9%-16%).
- IUGR.
- Fetal Distress.
- IUD or Still birth (4.7%-13%.).
- Increased incidence of caesarean deliveries.
- Post-Partum Haemorrhage (PPH).
New born presentation
- Fever
- Hepatomegaly
- Thrombocytopenia
- Circulatory insufficiency
Causes of Maternal death
- Sever Antepartum Hemorrhage (APH)
- Sever Post-partum Hemorrhage (PPH)
- Dengue shock syndrome (DSS)
- Multi organ failure (MOF)
Causes of Fetal death
- Fetal distress
- Fetal circulatory insufficiency
- Fetal coagulopathy
Fetal well-being evaluation
USG of pregnancy profile
- Gestational age
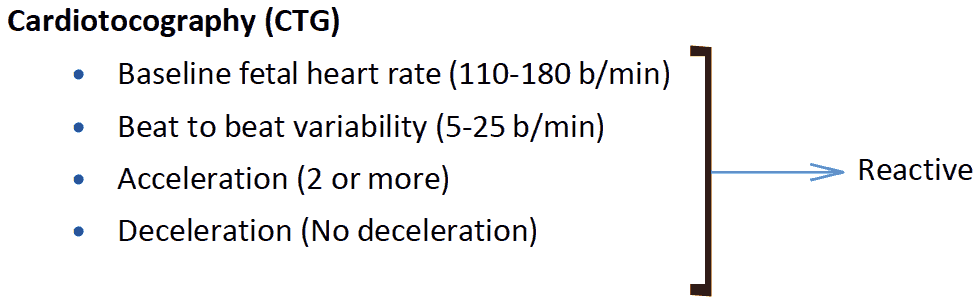
- Fetal Heart Rate (FHR)
- Fetal weight
- Fetal Presentation
- AFI
- Placental position and maturation
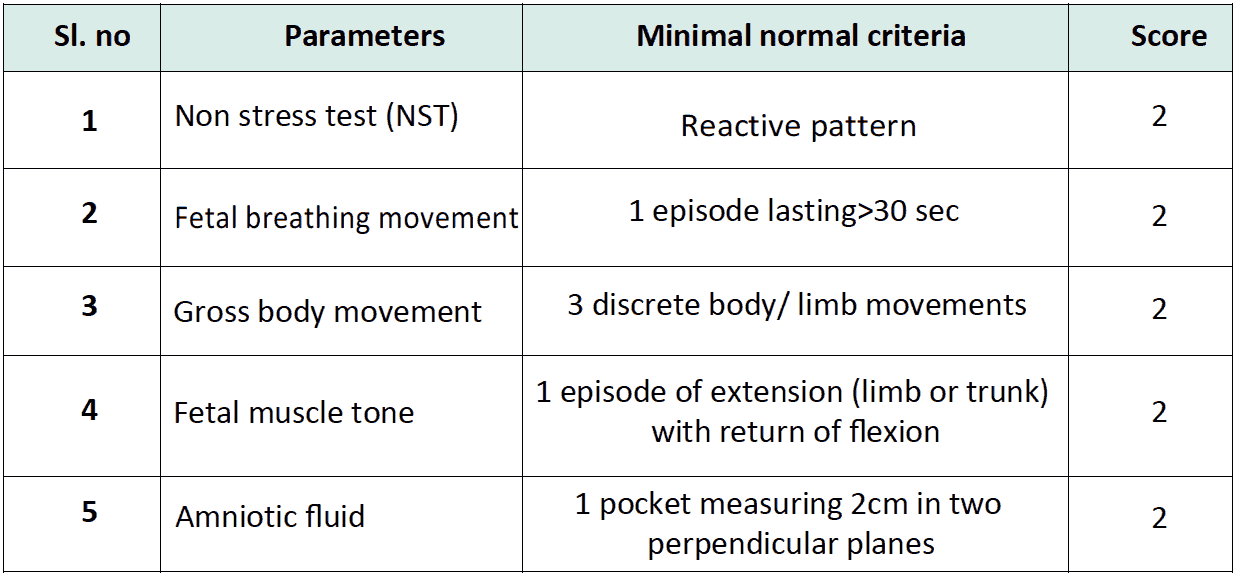
Biophysical profile
BPP Scoring interpretation and management
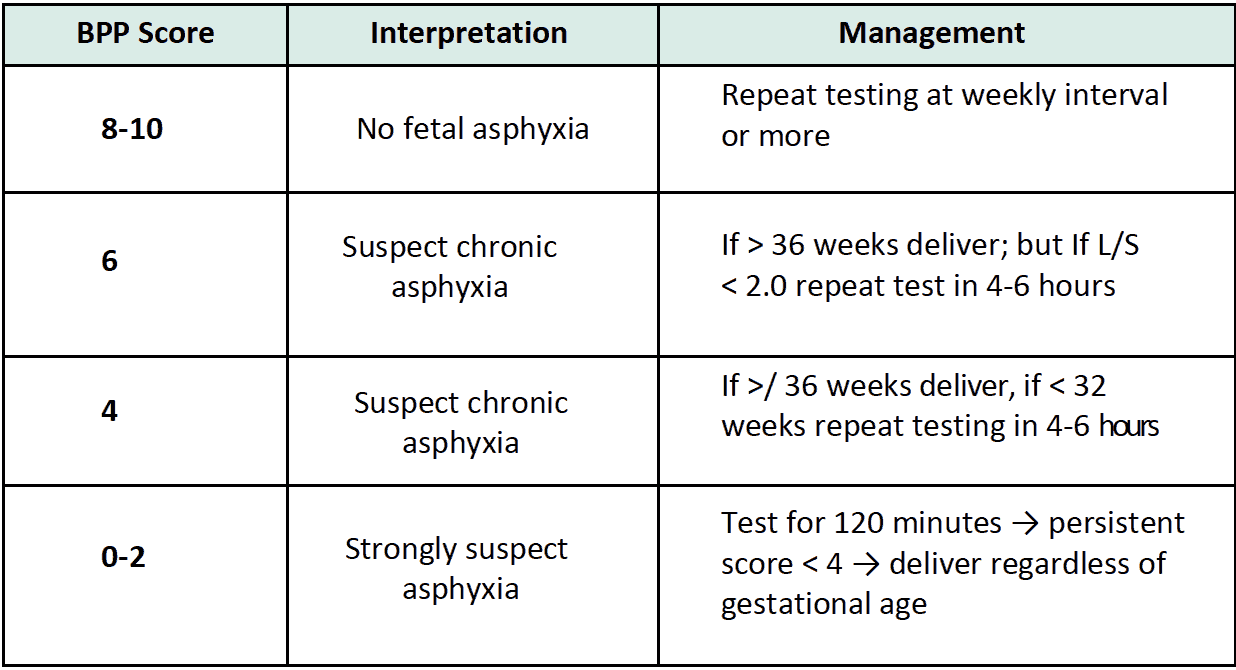
Note - When the patient in critical phase then we will try to delay the delivery to prevent complications.
Admission is required and close follow up with CBC daily is very important
The gestation and the phase of dengue are important factors in determining the management. A multi-disciplinary team consisting of obstetricians, physician, anesthetist and the paediatrician should get involved in the management.
- When a Suspected dengue (febrile patient) is first seen, look for warning signs and admit if anyone is found.
- If admitted to the obstetric ward urgent referral to the physician is essential.
- Explanation to the family members about the course of DHF and the management is important.
The signs, symptoms and lab investigations may be confused with other complications of pregnancy such as toxaemia and HELLP syndrome (Haemolysis, Elevated Liver Enzymes and Low Platelets). It is essential to consider the possibility of dengue in a patient with features of HELLP. Increased incidence of abruptio placentae, death in-utero and prematurity are reported.
Complication:
- Premature fetal loss or vertical transmission in Dengue infection may be one of the grave fetal complications in pregnancy.
- The vertical transmission in fetus is evidenced by fever, thrombocytopenia, raised liver enzymes, gastric bleeding, pleural effusion, convalescent rash and Dengue specific IgM (+).
- The important maternal complications include thrombocytopenia, raised liver enzymes, febrile illness, gum bleeding and bilateral pleural effusions.
- Moreover, uncomplicated pregnancy may be complicated with DHF.
- Delivery should be conducted in a tertiary hospital where all advanced facilities are available.
The normal physiological changes in pregnancy make the diagnosis and assessment of plasma leakage difficult. Therefore, the following baseline parameters should be noted as early as possible on the first day of illness:
- Pulse, blood pressure (BP), pulse pressure. (Baseline BP is often lower and pulse pressure wider & heart rate may be higher)
- CBC - (Haemoglobin, HCT & platelet count may be lower than in nonpregnant patient)
- SGOT/SGPT
- Clinical detection of pleural effusion and ascites may be difficult due to the presence of gravid uterus. Use of Ultra Sound Scan to detect the following, is advisable
- Pleural effusion
- Ascites (Gallbladder wall oedema may be seen in both DF & DHF)
Generally, the presentation and clinical course of dengue in pregnant women is similar to that in non-pregnant individuals. The fluid volume for the critical period (M+5%) for a pregnant mother should be calculated (based on the weight prior to pregnancy)
Management of pregnant patients with DF/DHF close to delivery
Risk of bleeding is at its highest during the period of plasma leakage (critical phase). Therefore, unless to save mothers life, avoid Lower uterine segment Caesarean Section (LUCS) or induction of labour during the Critical (plasma leakage) phase. Obstetric procedures (such as amniocentesis or external cephalic version) should be avoided during the illness. If obstetric procedures are to be undertaken,
- Maintain the platelet count above 50,000/mm3 Single donor platelet transfusion is preferred, if available.
- If patient goes into spontaneous labour during critical phase take steps to prevent vaginal tears by performing an episiotomy.
- In a case of fetal compromise priority should be given to the mother’s life and decision making should involve the multidisciplinary team.
- Counseling the family on the probable outcome is essential.
Management of patients with DF/DHF during immediate postpartum
Dengue fever should be suspected in patients having fever in the immediate post-partum period since this may be overlooked. Early referral to a physician is recommended.
