Chapter - 3: Blood Pressure Measurement
exp date isn't null, but text field is
Blood pressure should be measured correctly. Blood Pressure constantly varies and rises with stress, excitement and environment. To declare a patient as having hypertension may cause mental trauma, so think more to declare to have hypertension & be empathetic to the patient. There are four common devices used for the measurement of BP namely, (a) mercury column sphygmomanometer, (b) aneroid sphygmomanometer, (c) electronic devices and (d) automated ambulatory BP monitoring devices. The mercury and aneroid sphygmomanometer are gradually being replaced by the electronic blood pressure measurement device due to interobserver variation, environmental and health concerns. There are many calibrated electronic or ambulatory BP devices available in the market. Only professionally validated electronic models should be used.
3.1 Office or clinic blood pressure measurement
The measurement of BP in the office or clinic is most commonly the basis for hypertension diagnosis and follow-up. Care should be taken to follow the correct procedures regarding arm position, posture of the patient, cuff size and the number of readings that should be taken. Instructions for correct office blood pressure measurements are summarized in Box 1. Validated electronic (oscillometric) upper-arm cuff devices are recommended for measurement of clinic or office BP. Lists of accurate electronic devices for office, home and ambulatory BP measurement in adults, children and pregnant women are available at www.stridebp.org. Alternatively use a calibrated auscultatory device, (aneroid, or hybrid devices). Use of mercury sphygmomanometers is discouraged due to environmental pollution by mercury.
3.2 Self or ambulatory BP monitoring
If possible and available, the diagnosis of hypertension should be confirmed by out-of-office BP measurement9,11. Although recent guidelines have recommended the use of self BP monitoring (SBPM) and ambulatory BP monitoring (ABPM) for diagnosis of hypertension, the guideline expert group recommend using clinic blood pressure for diagnosis of elevated blood pressure taking considering the resources constrain for acquiring appropriate device and other logistics by the health care providers and patients. However, SBPM and ABPM are recommended in specific circumstances for selected target groups. For more information, see Annexure 1.
Box 1
Recommendations for office blood pressure measurement
Conditions
- Ensure quite room with comfortable temperature.
- Patients should avoid tobacco, caffeine-containing beverages (tea or coffee), or exercise in the preceding 30 minutes of BP Patients should also have an empty bladder.
- Neither the patient nor staff should talk before, during and between BP measurement.
- Patient should not read or use mobile before, during and between BP measurement.
Position
- Patient should be seated for at least 5 minutes before measurement.
- During measurement patient should be seated with the back supported, leg uncrossed, feet flat and parallel on floor.
- Arm should be resting on a surface at heart-level. Bare arm preferred. Take off thick or excess clothing, roll up long sleeves, ensure rolled up sleeve is not too tight on the upper arm. In some circumstances bare arm is not practical, in that case thin clothing may be accepted.
Device
- Validated electronic (oscillometric) upper-arm cuff device.
- Alternatively use a calibrated auscultatory device, (aneroid, or hybrid as mercury sphygmomanometers are banned in most countries) with 1st Korotkoff sound for systolic blood pressure and 5th for diastolic with a low deflation rate.
Cuff
- Size according to the individual’s arm circumference (smaller cuff overestimates and larger cuff underestimates blood pressure). Use a standard bladder (12–13 cm long and 35 cm wide) but have a larger and a smaller bladder available for fat and thin arms, respectively. Use smaller bladder in children.
- Find the pulse at the bend in the elbow. Make sure to align the ‘Arrow’ on the cuff directly over it.
- Cuff should be wrapped snugly and fasten with Velcro. There should be enough space to slip two fingers under the bottom edge of the cuff.
- Cuff should cover most of the upper arm leaving a gap of about 1 cm below the axilla and 2-3 cm above the antecubital fossa. Use standard cuff size for adult and pediatric patient, which is available in the market.
- For manual auscultatory devices, cuff and sphygmomanometer should be placed at heart level and the inflatable bladder of the cuff must cover 75%–100% of the individual’s arm circumference.
- For electronic devices use cuffs according to device instructions. Have the cuff at the heart level, whatever the position of the patient.
Protocol
- Measure BP in both arms at first visit to detect possible differences. In this instance, take the higher value as the reference one.
- If BP of first reading is <130/85 mmHg no further measurement is required. If value is higher, ≥130/85 mmHg, measure two more BP in higher value arm with 1 min between them. Calculate the average of the last 2 measurements for diagnosis.
- Before measuring BP, history should be taken. BP should not be taken from an arm with arteriovenous fistula, for fear of damaging the fistula and should not be measured using the arm on the side of previous mastectomy for fear of upsetting the lymphatic drainage.
For electronic (oscillometric) upper-arm cuff device
- Turn the monitor on from the on/off button.
- Place the cuff in accurate position as stated above section.
- Press the START/STOP button to begin the measurement.
- The BP cuff will start to inflate. During inflating, a pressure or tightness may appear on the arm. This might be uncomfortable for some. Reassure the patient that the pressure or tightness on the arm is temporary.
- The cuff will deflate slowly.
- When the systolic and diastolic readings and pulse rate will appear on the screen/monitor, the reading is complete.
- If the monitor/machine does not record the reading, Reconnect the cuff with the device and check the battery or power supply of the device. Then reposition the cuff on upper arm and try again after 1-2 minutes and repeat the above-mentioned steps.
- Regarding Blood pressure readings record the actual measurements shown in the screen.
- Turn the machine off and remove the cuff.
- Please ensure, to deflate the cuff of an electronic or digital BP device, never squeeze the cuff, as the sensor in the cuff may be damaged.
For Aneroid or Mercury BP device use
- If auscultatory device used, (aneroid, or hybrid or mercury sphygmomanometers in most countries) SBP should be estimated first by palpation to avoid missing the auscultatory gap.
- The manometer should be at the same level of the cuff (if aneroid BP machine is used) on the patient’s arm, Centre of the bladder (not the cuff) should be placed over the brachial artery.
- Place the stethoscope lightly over the brachial artery, slipped underneath the distal end of the cuff.
- Palpate the radial pulse while inflating the cuff to a level of 20-30 mmHg above the level at which radial pulse can no longer be felt. Then deflate the bladder slowly 2-3 mmHg/sec until you have a regular tapping sound.
- Systolic and diastolic BP should be recorded with 1st and 5th Korotkoff sound respectively with a low deflation rate (2 mmHg per second).
Interpretation
- Blood pressure of 2–3 office visits ≥140/90 mmHg indicates hypertension.
- Record the blood pressure which is higher and mentioning the site (right/left arm) for future follow up.
- Provide patient the SBP/DBP reading both verbally and in writing.
- Write BP with mentioning where and how it is recorded e. g- 120/60 mmHg, left/right arm, sitting/supine.
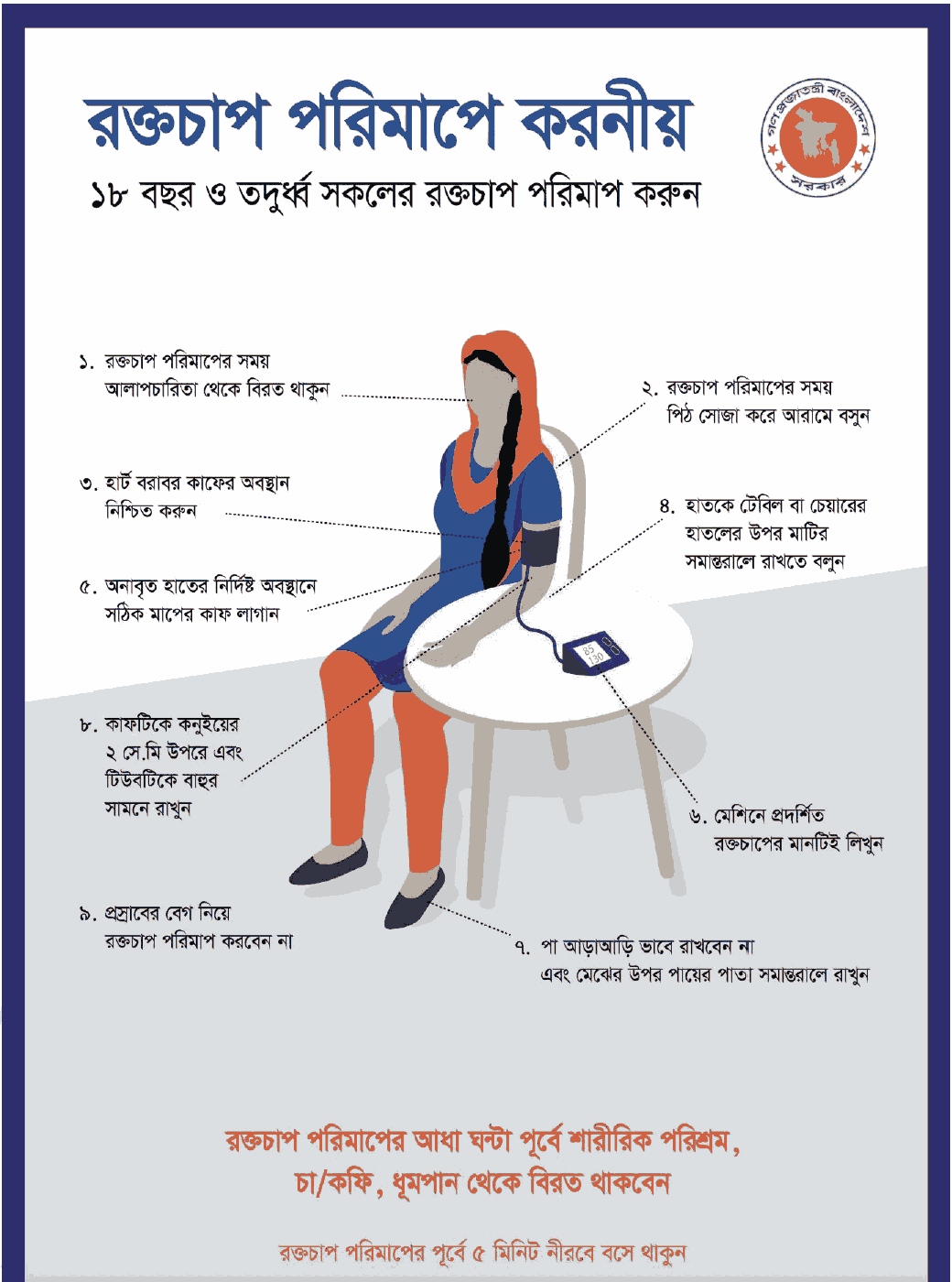
Figure 1: Measures should be followed during BP measurement.
Leg Blood Pressure
- A large cuff (45-52cm long) other than traditional standard cuff (35-44 cm long) is placed over the mid-thigh. Patient lies prone and the stethoscope is placed in the popliteal fossa, behind the knee. Leg BP is normally higher than arm pressure (up to 20 mmHg higher).
- Ankle BP is measured in a supine position, using a cuff placed around the ankle/lower calf ensuring the bladder encircles ≥80% of the ankle circumference. Readings should be taken either by oscillometry or Doppler readings of return to flow at the dorsalis pedis or posterior tibial arteries (systolic readings only). Auscultation is not feasible in most subjects and is not therefore recommended. Ankle BPs are recommended rather than calf or thigh measurements because they generally cause less discomfort and the cuff is easier to fit, particularly in obese patients. As with standard clinic BP measurement, readings should be taken after a 5-min rest period. An ankle BP threshold of ≥155/90 mmHg to define high blood pressure in patients who do not have vascular disease15.
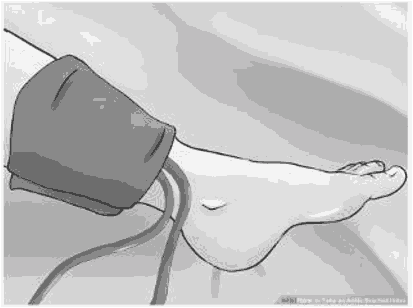 Figure 2: Positioning of the blood pressure monitoring cuff on the ankle/ lower calf.
Figure 2: Positioning of the blood pressure monitoring cuff on the ankle/ lower calf.
Image taken from Wiki How to take an Ankle Brachial Index
(https://www.wikihow.com/Take-an-Ankle-Brachial-Index)
