4.1 Diagnosis
exp date isn't null, but text field is
The diagnosis of hypertension should be based on multiple blood pressure measurements, taken on separate occasions over a period. BP can be highly variable; thus, the diagnosis of hypertension should not be based on a single set of BP readings at a single office visit. In general, the diagnosis of hypertension should be based on at least three blood pressure measurements per visit and at least two to three visits at 1–4-week intervals (depending on the BP level) to confirm the diagnosis of hypertension9.
The diagnosis might be made on a single visit, if BP is ≥160/100 mmHg or there is accompanying evidence of hypertension mediated organ damage (HMOD) (e.g., hypertensive retinopathy with exudates and hemorrhages, or LVH, or vascular or renal damage)10. When the initial SBP is between 140 and 159 mmHg, or the DBP is between 90 and 99 mmHg, repeat measurements should be performed on three separate occasions within a period of 1 to 4 weeks to determine whether a diagnosis of hypertension is valid. All measurements should be taken in the same arm. If possible and available, the diagnosis of hypertension should be confirmed by out-of-office BP measurement (i.e., HBPM and/or ABPM)9.
In the initial evaluation, measurement of blood pressure should be performed in both arms. If the difference in readings between arms is more than 10 mmHg, repeat the measurements at 1-2 mins interval. If the difference in readings between arms remains more than 10 mmHg on the second measurement, measure subsequent blood pressures in the arm with the higher reading and it should be noted. If the difference is >20 mmHg, consider further investigation9.
If hypertension is not diagnosed, measure the person's clinic blood pressure at least every 3 years subsequently, and consider measuring it more frequently if the person's clinic blood pressure is close to 140/90 mmHg (Table 3).
|
Table 3. Blood Pressure Measurement Plan According to Office Blood Pressure Levels10 |
||
|
Office Blood Pressure Levels (mmHg) |
||
|
<130/85 |
130–159/85–99 |
>160/100 |
|
Remeasure within 3 years (1 year in those with other risk factors) |
Confirm with repeated office visits. If possible, confirm with out of office BP measurement |
Confirm within a few days or weeks |
Postural Hypotension16:
Patient should lie down for 5 minutes, and measure BP and pulse rate. Then have the patient stand and repeat BP and pulse rate measurements 1 and 3 minutes after standing. A drop in SBP of ≥20 mmHg, or in DBP of ≥10 mmHg, or experiencing lightheadedness or dizziness on standing is considered abnormal and indicates postural hypotension.
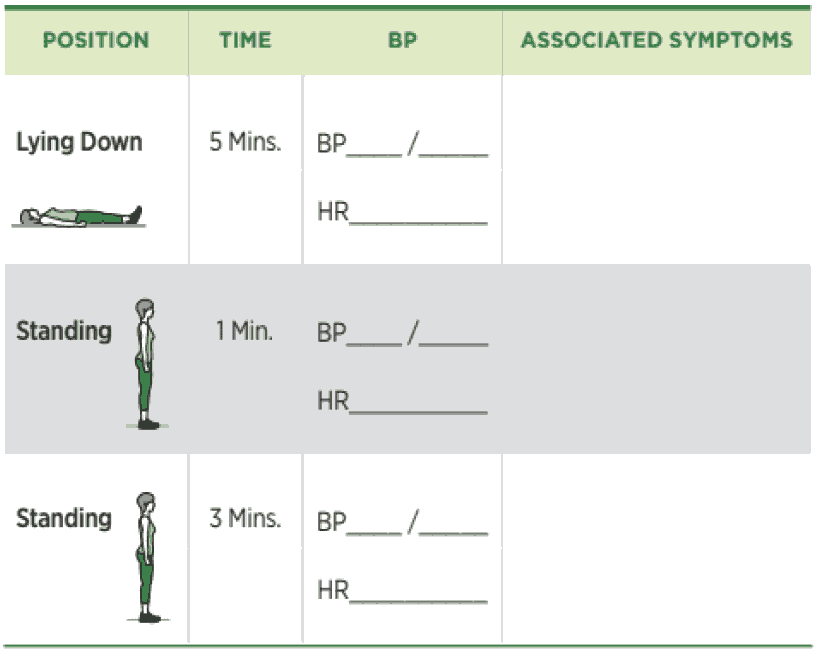
Measure standing blood pressure in treated hypertensives with symptoms of postural hypotension (falls or postural dizziness) and at the first visit in the elderly and people with diabetes. BP is to be measured first in supine or seated position, and again with the person standing for at least 1 minute prior to measurement. If the systolic BP falls by ≥ 20 mmHg when the person is standing, medication is to be reviewed, subsequent BP is to be measured with the person standing and the patient may be referred to specialist care if symptoms of postural hypotension persist.
