The goals of the initial evaluation of the hypertensive patient are to
- Establish the diagnosis and grade of hypertension.
- Screening for potential secondary causes of hypertension.
- Identify factors that potentially contribute to development of hypertension (lifestyle, concomitant medications, or family history).
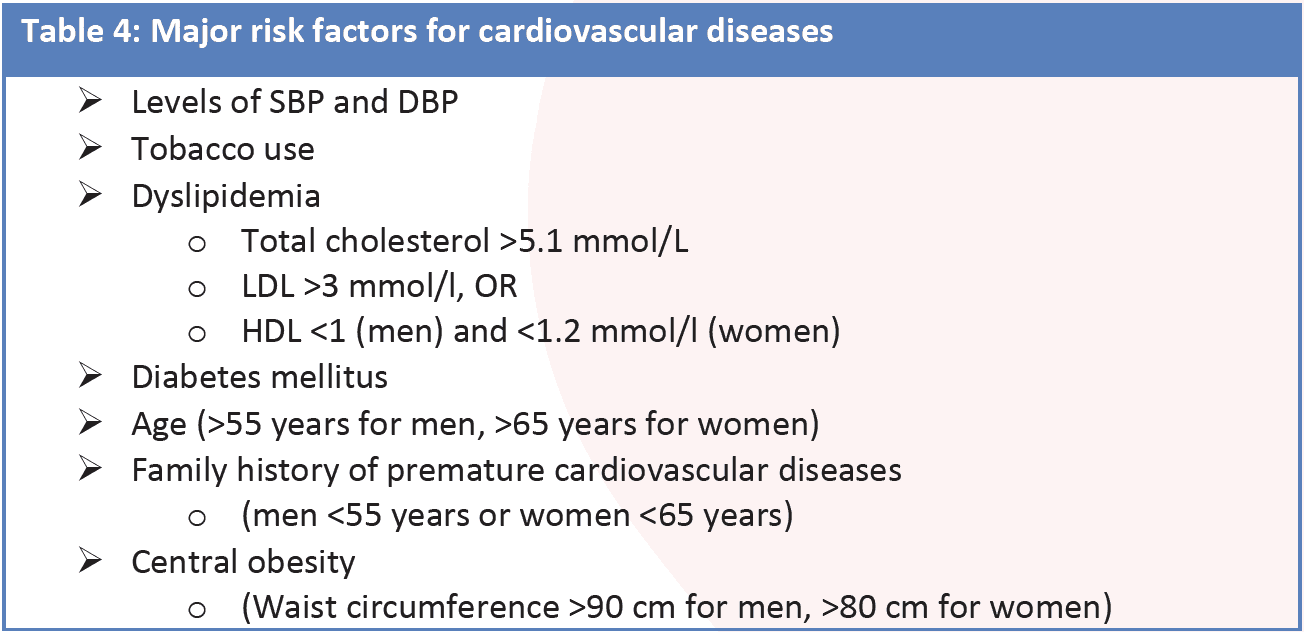
- Identify concomitant CV risk factors (including lifestyle and family history) (Table 4)
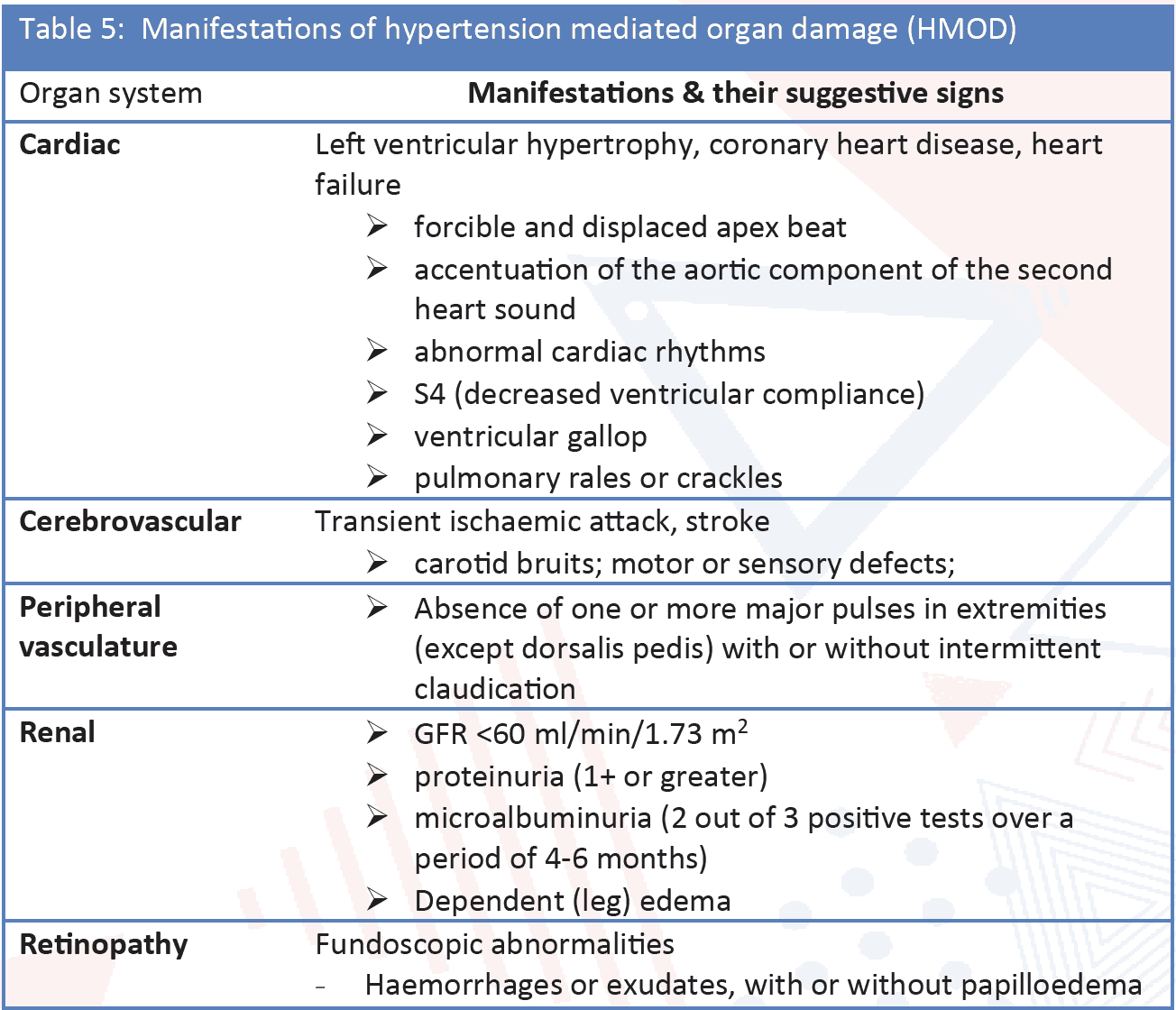
- Identify concomitant diseases and establish whether there is evidence of HMOD or existing cardiovascular, cerebrovascular, or renal disease. (Table 5)
These goals are usually accomplished by a thorough medical history, physical examination, and simple laboratory investigations. While waiting for confirmation of a diagnosis of hypertension, carry out some routine investigations for assessment of HMOD. If hypertension is not diagnosed but there is evidence of HMOD, consider carrying out investigations for alternative causes of HMOD.
History
Most patients with hypertension are asymptomatic, the high blood pressure usually having been noted during an incidental clinical examination. A proportion of patients will present with a major complication of hypertension such as stroke or myocardial infarction, but only a small number will present with symptoms directly attributable to hypertension such as breathlessness or headache. That is why hypertension is called a ‘Silent killer’. The key issues that need to be addressed in the history include:
Risk factors assessment:
- Family and personal history of hypertension, CVD, stroke, or renal disease.
- Family and personal history of associated risk factors (e.g., familial hypercholesterolaemia)
- Dietary history and salt intake
- Smoking history
- Alcohol consumption
- History of physical exercise/sedentary lifestyle
- History of erectile dysfunction
- Sleep history, snoring, sleep apnoea (information also from partner)
- Previous hypertension in pregnancy/pre-eclampsia
- History of oral contraceptive use
History of symptoms of HMOD, CVD, stroke, and renal disease
- For Brain and eyes: headache, vertigo, syncope, impaired vision, TIA, sensory or motor deficit, stroke, carotid revascularization, cognitive impairment, dementia (in the elderly).
- Heart: chest pain, shortness of breath, oedema, myocardial infarction, coronary revascularization, syncope, history of palpitations, arrhythmias (especially AF), heart failure.
- Kidney: thirst, polyuria, nocturia, haematuria, urinary tract infections.
- Peripheral arteries: cold extremities, intermittent claudication, pain free walking distance, pain at rest, peripheral revascularization, patient or family history of CKD (e.g., polycystic kidney disease).
History of Antihypertensive Drug Treatment
- Current/past antihypertensive medication including effectiveness, intolerance or side effects of previous medications.
- Adherence to therapy and in non-compliant patients the reason behind it (including financial constraint).
Physical Examination
The physical examination should include the following:
- Weight and height measured on a calibrated scale, with calculation of BMI
- Waist circumference
- Neurological examination and cognitive status
- Fundoscopic examination for hypertensive retinopathy
- Palpation and auscultation of heart and carotid arteries
- Palpation of peripheral arteries
- Comparison of BP in both arms (at least once)
- Skin inspection: cafe-au-lait patches of neurofibromatosis (phaeochromocytoma)
- Kidney palpation for signs of renal enlargement in polycystic kidney disease
- Auscultation of heart and renal arteries for murmurs or bruits indicative of aortic coarctation, or renal artery stenosis
- Comparison of radial with femoral pulse: to detect radio-femoral delay in aortic coarctation
- Signs of Cushing’s disease or acromegaly
- Signs of thyroid disease