The ideal drug for treatment of hypertension must be efficacious, free from side-effects, able to prevent all the complications of hypertension, easy to use and affordable. Affordability is an important issue for maintaining compliance with treatment as many patients in Bangladesh would need to pay out of their own pocket for this chronic condition. Therefore, the guideline committee strongly reiterates the importance of lifestyle modification at all stages of hypertension. Currently, the price of antihypertensive and other drugs fluctuates considerably. Where possible, generic equivalents and combinations are encouraged and the cheapest generic in a class should be considered if it is a true equivalent. The drug should not be changed frequently from one generic to another in the same class, solely because of lower price. Best practice recommendations should be followed but compromises, based on limited resources, should be made deliberately and transparently.
5.3 Pharmacological Management
exp date isn't null, but text field is
The following must be considered prior to the selection of an antihypertensive agent: the cost of the drug class, patient-related factors such as the presence of major risk factors, conditions favoring use, contraindications and HMOD. For adults with hypertension requiring pharmacological treatment, guideline committee recommends the use of drugs from any of the following five classes of pharmacological antihypertensive medications as an initial treatment: ACE inhibitors, ARBs, beta-blockers, CCBs, and diuretics (thiazides and thiazide-like diuretics such as chlortalidone and indapamide)9,11.
Guidelines have generated a variety of different strategies to initiate and escalate BP lowering medication to improve BP control rates. In previous Guidelines, the emphasis was on initial use of different monotherapies, increasing their dose, or substituting for another monotherapy. However, increasing the dose of monotherapy produces little additional BP lowering and may increase the risk of adverse effects, whilst switching from one monotherapy to another is frustrating, time consuming, and often ineffective. For these reasons, most recent Guidelines have increasingly focused on the stepped- care approach, initiating treatment with different monotherapies and then sequentially adding other drugs until BP control is achieved. Figure 4 outlines the management approach for starting treatment with monotherapy or free combination therapy of a patient with hypertension10.
Despite this widely followed stepped care approach, BP control rates have remained poor worldwide. Therefore, for adults with hypertension requiring pharmacological treatment, WHO recommended to start with combination therapy, preferably with a single-pill combination (SPC) (to improve adherence and persistence), as an initial treatment (Fig 5). Antihypertensive medications used in combination therapy should be chosen from the following three drug classes: diuretics (thiazide or thiazide-like), angiotensin-converting enzyme inhibitors (ACEis) /angiotensin-receptor blockers (ARBs), and long-acting dihydropyridine calcium channel blockers (CCBs).
Following drug treatment algorithm has been developed to provide a simple and pragmatic treatment recommendation for the treatment of hypertension, based on a few key recommendations11.
The initiation of treatment in most patients with a single-pill combination (SPC) comprising two drugs, to improve the speed, efficiency, and predictability of BP control.
- Preferred two-drug combinations are a RAS blocker with a CCB or a diuretic. A betablocker in combination with a diuretic or any drug from the other major classes is an alternative when there is a specific indication for a beta-blocker, e.g., angina, post myocardial infarction, heart failure, or heart rate control.
- Use monotherapy for low-risk patients with stage 1 hypertension whose SBP is <150 mmHg, very high-risk patients with high–normal BP, or frail older patients.
- The use of a three-drug SPC comprising a RAS blocker, a CCB, and a diuretic if BP is not controlled by a two-drug SPC.
- The addition of spironolactone for the treatment of resistant hypertension, unless contraindicated.
- The use of other classes of antihypertensive drugs in the rare circumstances in which BP is not controlled by the above treatments.
Fig 4. Algorithm 1: An approach for starting treatment with monotherapy or free combination therapy10. (Adapted from WHO 2021)
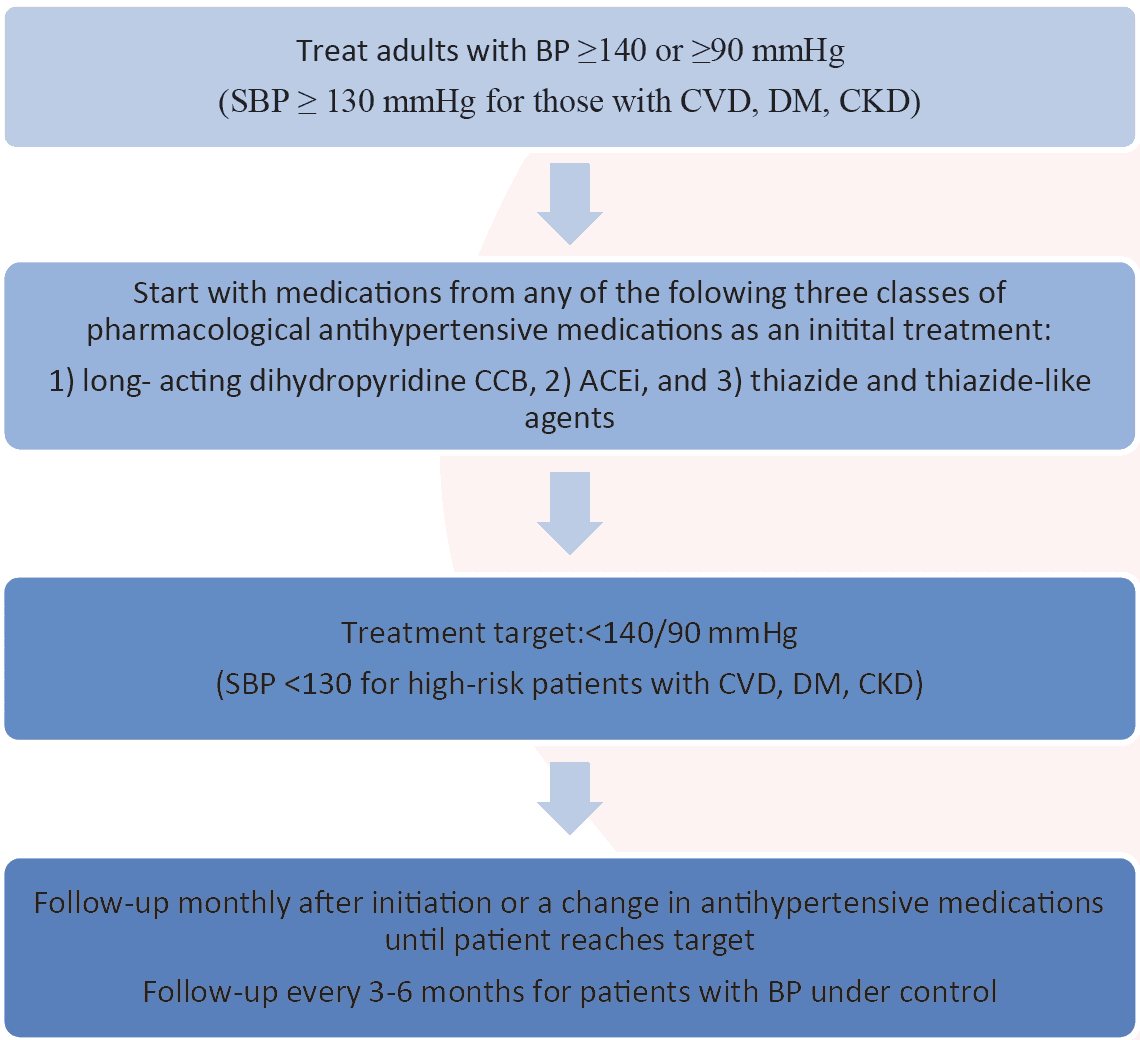
Pharmacological treatment to be initiated under the following circumstances:
A diagnosis of HTN has already been made.
Initiation of pharmacological HTN treatment should start no later than four weeks after diagnosis of HTN.
If BP level is high or there is accompanying evidence of end organ damage, initiation of treatment should be started without delay.
Patient should be counselled about starting medication therapy.
Basic laboratory testing (electrolytes, creatinine, lipogram, glucose, HbA1C, urine dipstick, and ECG) to occur if it does not delay treatment.
A cv risk assessment can be conducted immediately (as long as it does not delay initiation of treatment or at later visit)
A CCB, rather than a thiazide-type diuretic or ACEi/ARB, should be selected as first-line medication if one agent is used, to avoid the need for electrolyte measurements or to alleviate concerns regarding potential change in GFR.
Drugs affecting the renin-angiotensin system (ACEis, ARBs, and aliskiren) have been associated with serious fetal toxicity, including renal and cardiac abnormalities and death; they are contraindicated for use during pregnancy.
Consider using diuretic or CCB in patients 65 years or older, beta-blockers (BBs) in post MI, ACEis / ARBs in those with DM, heart failure or CKD.
Fig 5. Algorithm 2: Initiation of treatment with monotherapy or free combination therapy10
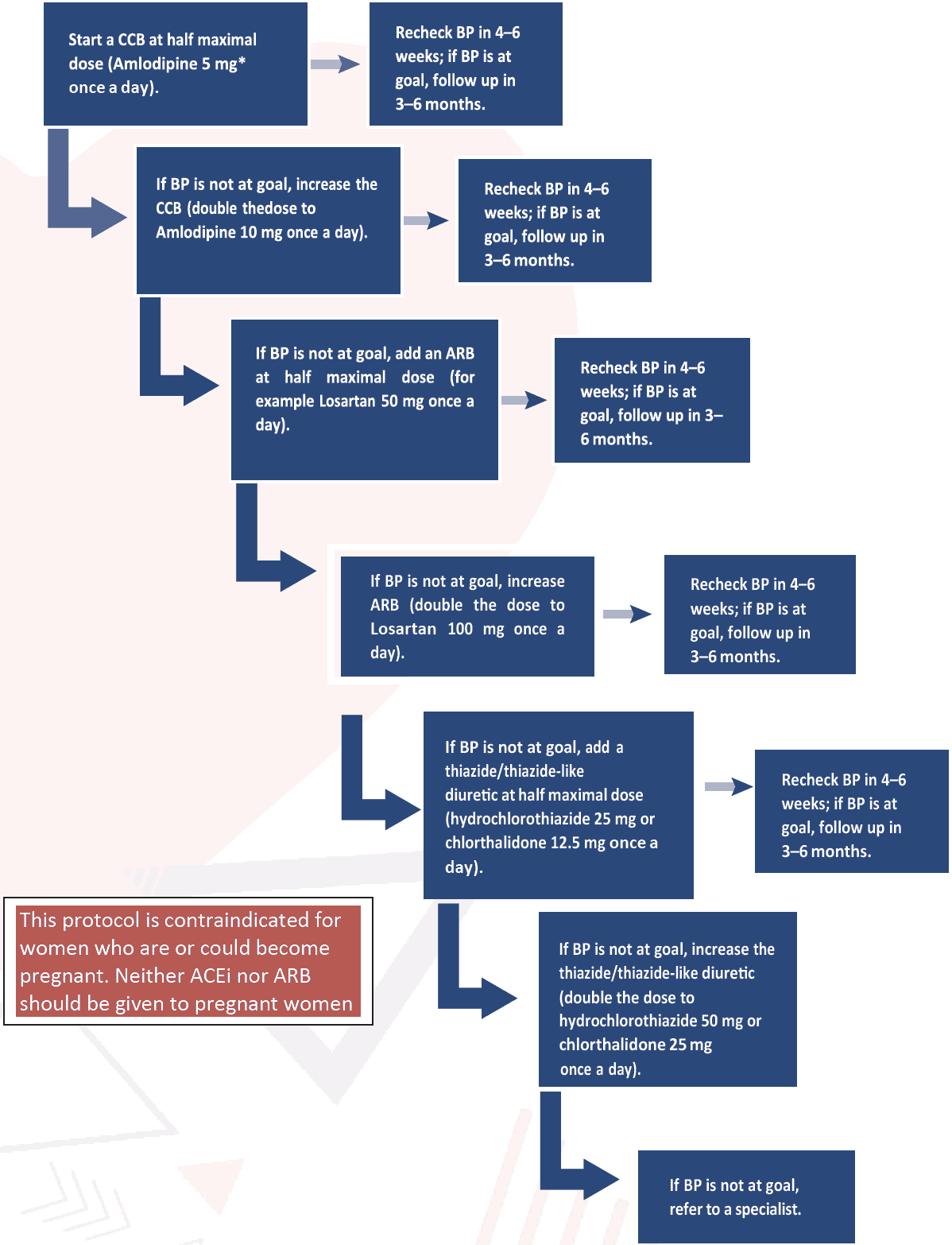
* Can be replaced with a thiazide/thiazide-like diuretic or an ACEi or ARB. An ACEi or ARB is preferred for proteinuria
Note: Monitor potassium and kidney function when starting or changing dose of ACEi/ARB or thiazide/thiazide-like diuretic, if testing is readily available and does not delay treatment.
Fig 6. Algorithm 3: An approach for starting treatment with single-pill combination (SPC)10
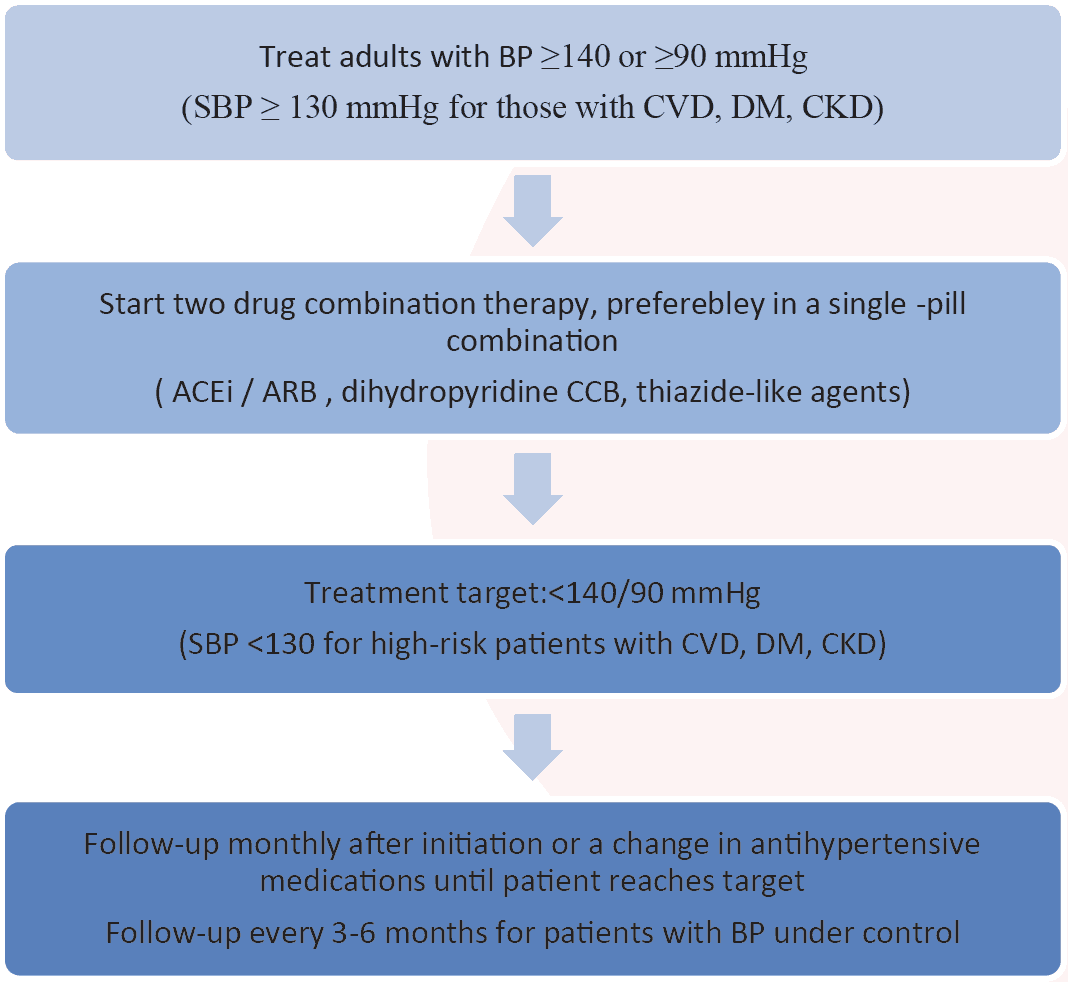
Fig 7. Algorithm 4: Initiation of treatment with a single-pill combination10
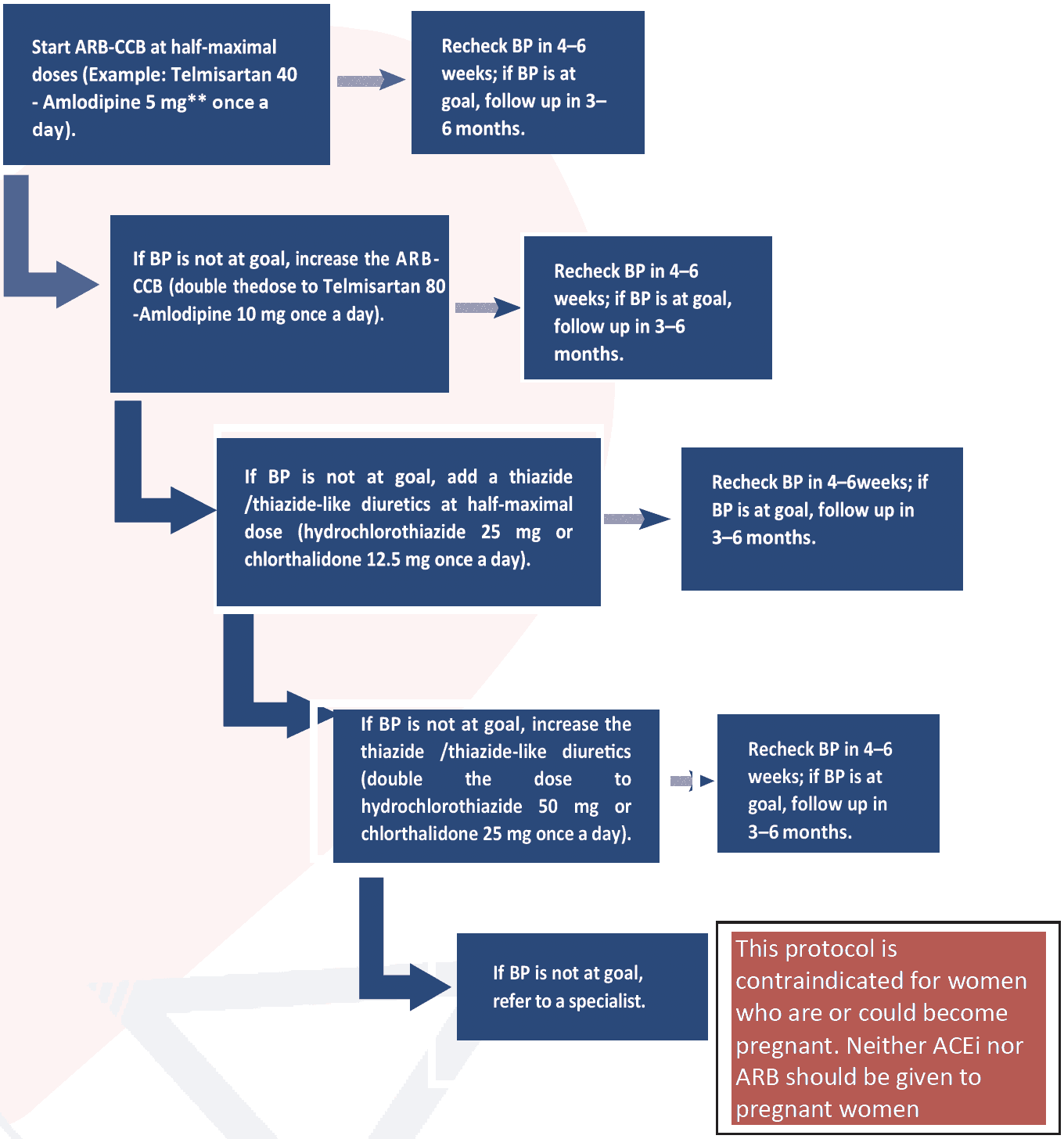
Note: Monitor potassium and kidney function when starting or changing dose of ACEi/ARB or thiazide/thiazide-like diuretic if testing is readily available and does not delay treatment.
*The medications mentioned serve as examples and can be replaced with any two medications from any of the three drug classes (ACEis/ARBs, CCBs or thiazide/thiazide-like diuretics). Start two individual pills or, if available, both in a single-pill combination (fixed-dose combination).
** Can be replaced with other individual pills or, if available, other single-pill combinations (fixed dose combinations).
An expert group convened by Non communicable Disease Control Programme of Directorate General of Health Services has developed a protocol for diagnosis and management of hypertension at primary care level in 2017 (Fig 7)14. Currently, an adapted version of this protocol is being used at NCD corners of all Upazila Health complexes (Fig. 8).
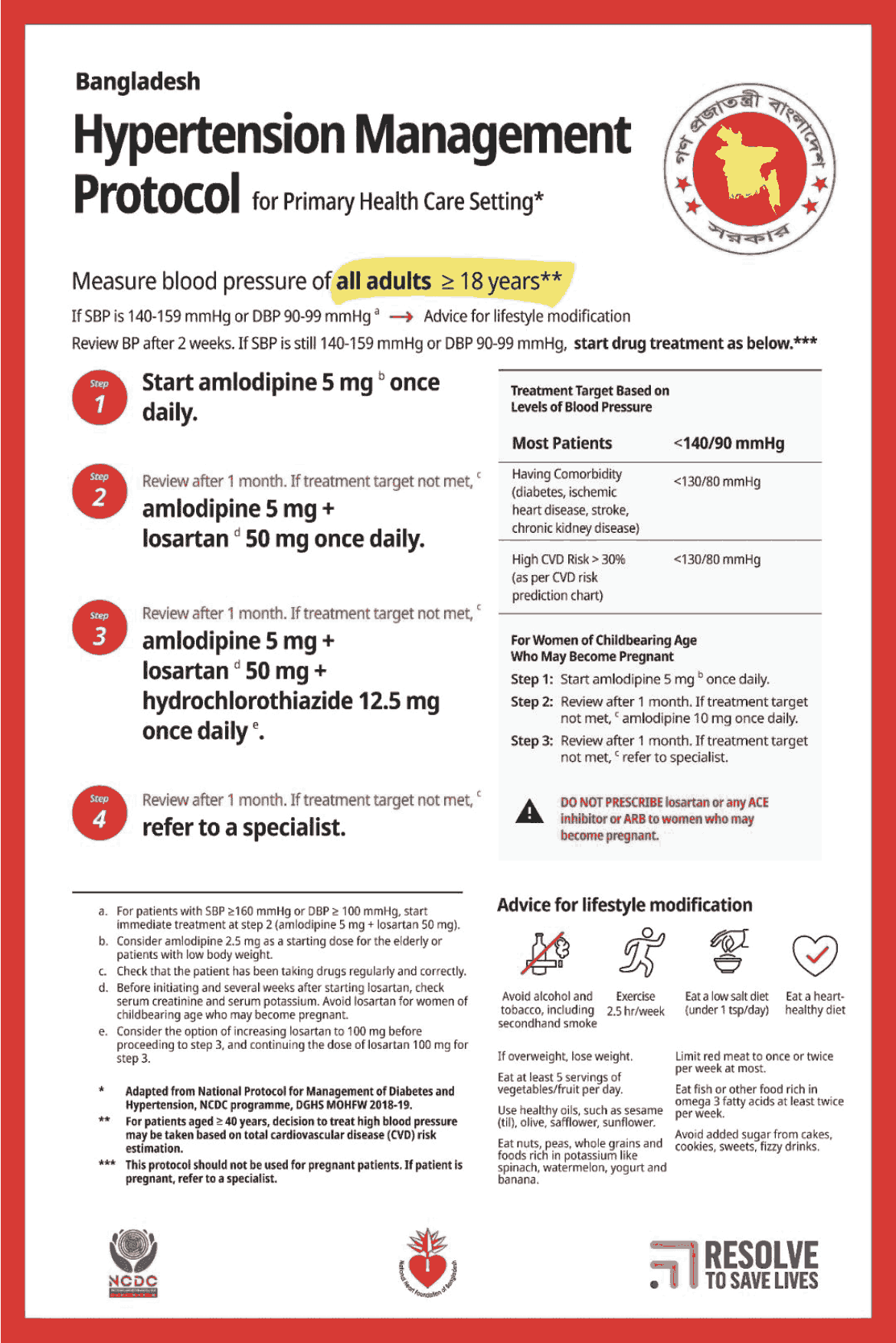
Figure 8: Hypertension Management Protocol at Primary Health Care Settings adapted from NCDC, DGHS, MOHFW
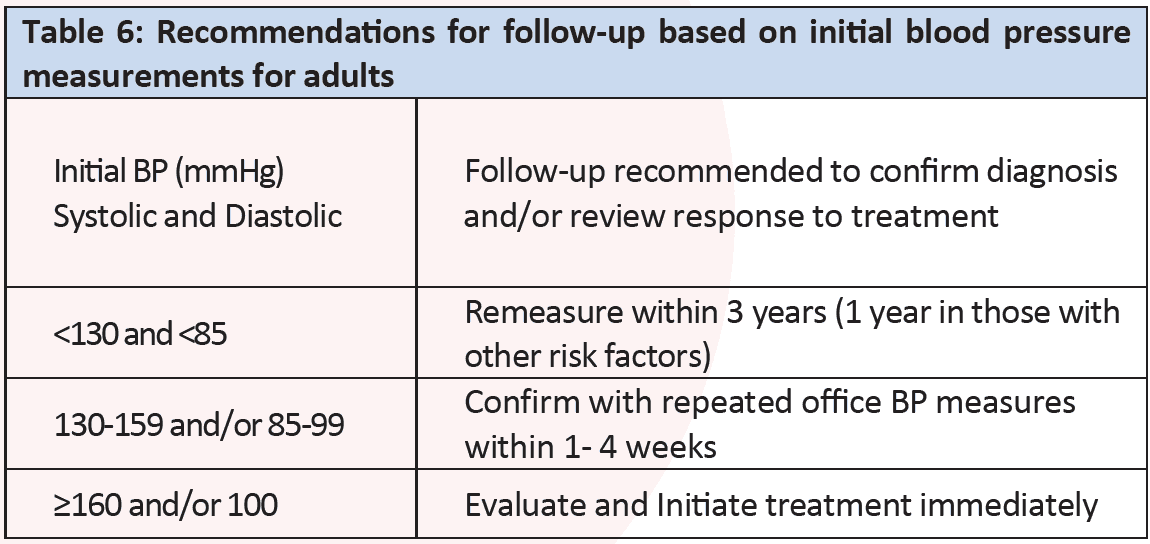
A monthly follow up after initiation or a change in antihypertensive medications until patients reach target should be done. Once target BP is achieved, follow-up at three to six- month interval is appropriate. Recommended blood pressure measurement plan according to office blood pressure levels is as shown in Table 6.
Efforts must be made to reach the target BP level. These targets should be reached within 3 months. In general, once the BP is controlled, most patients will require life-long treatment.
- A target blood pressure treatment goal of <140/90 mmHg in all patients with hypertension without comorbidities.
- A target systolic blood pressure treatment goal of <130 mmHg in high-risk patients with hypertension (those with high CVD risk, known CVD, diabetes mellitus, chronic kidney disease)10.
Patients with the following conditions should be referred to the appropriate specialist for further assessment. Indications for referral to the appropriate specialist include:
- accelerated or malignant hypertension
- suspected secondary hypertension
- resistant hypertension
- recent onset of target organ damage
- pregnancy
- children <18 years old
