Management50, 52-56
Overall Goals in management of pediatric HTN:
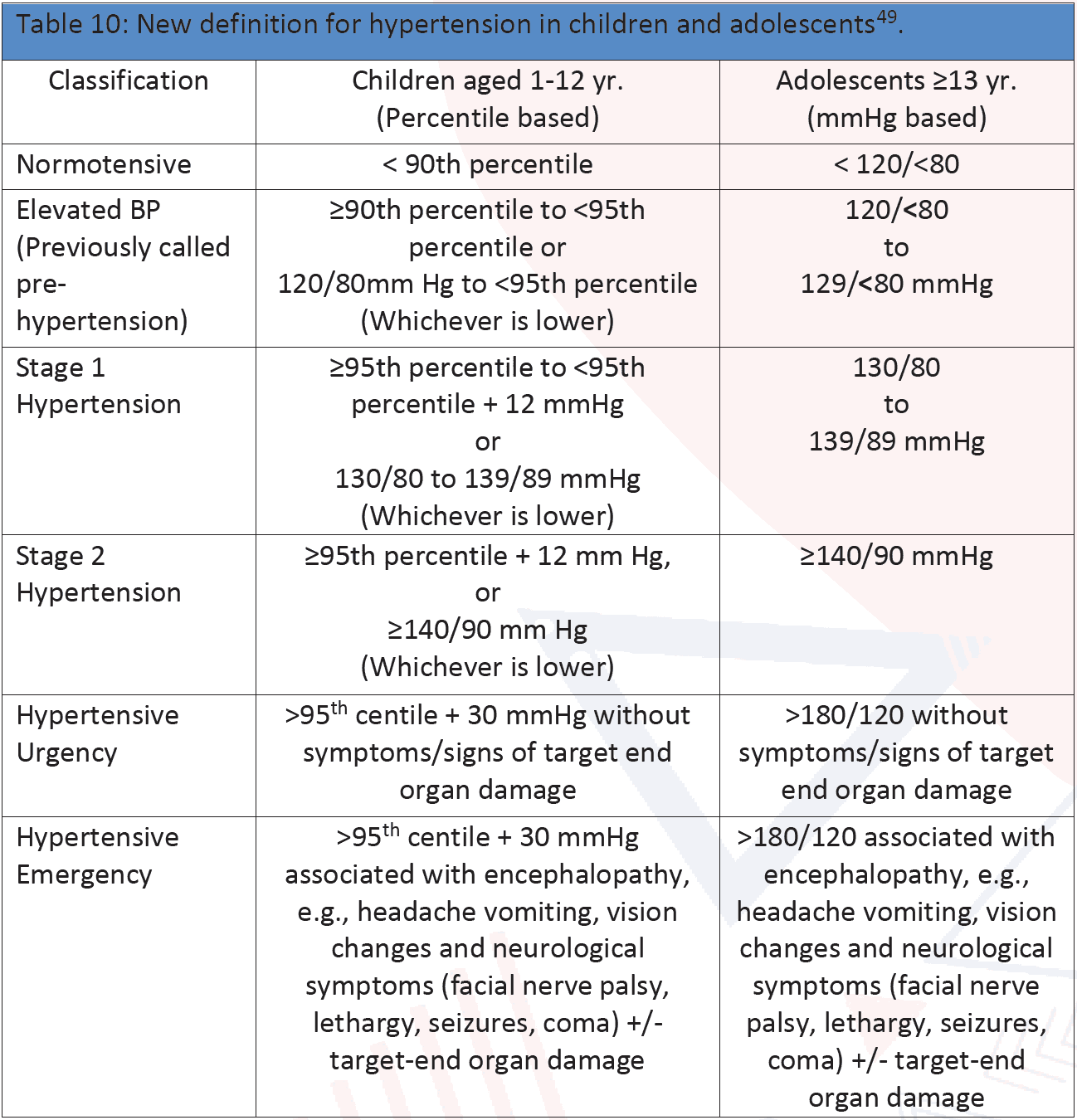
Overall Goals in management of pediatric HTN: An optimal BP level to be achieved with treatment of childhood HTN <90th percentile or <130/80 mm of Hg whichever is lower. Management should be started with history, physical examination and appropriate investigations.
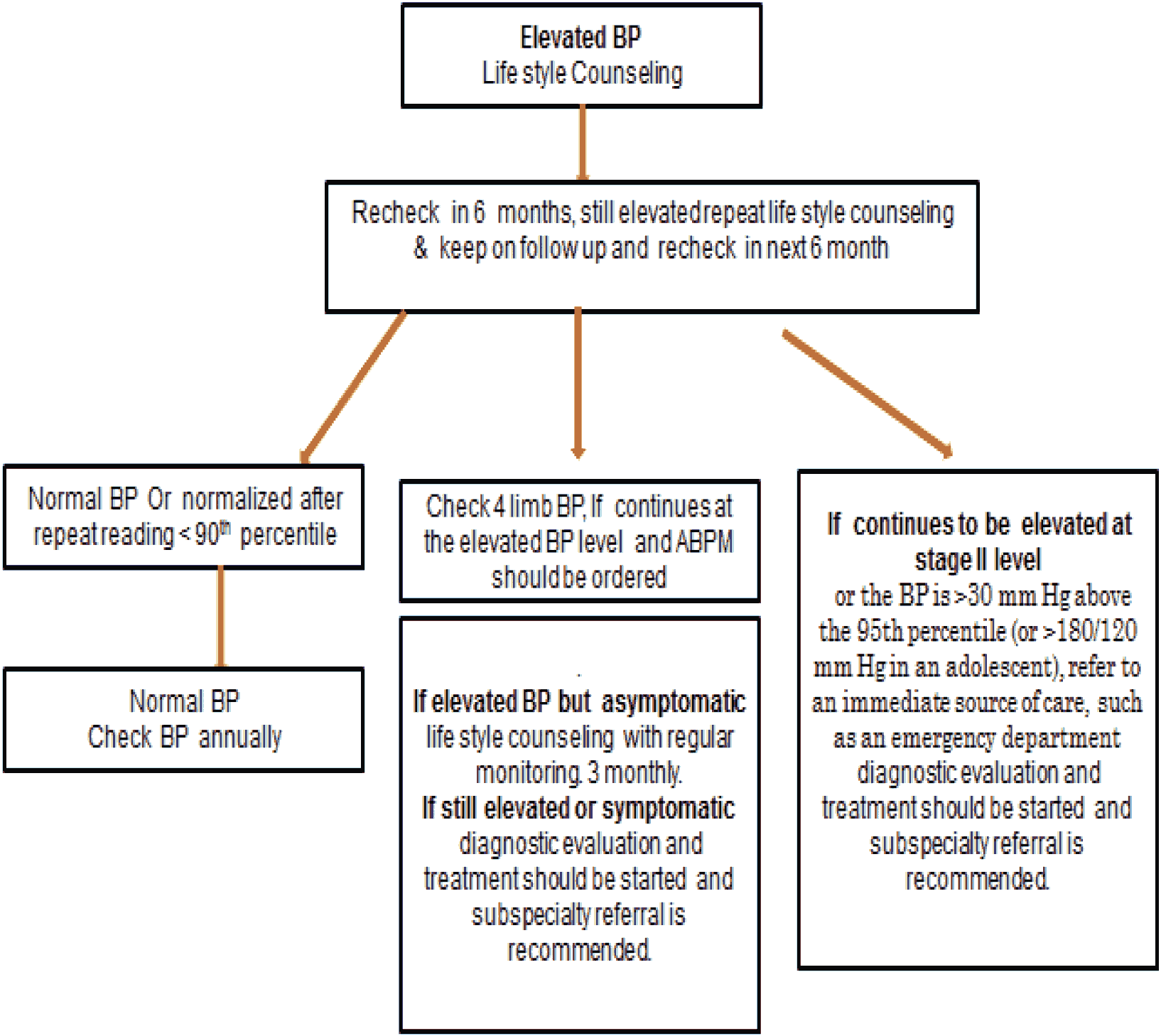
1. Lifestyle and Non-pharmacologic Interventions:
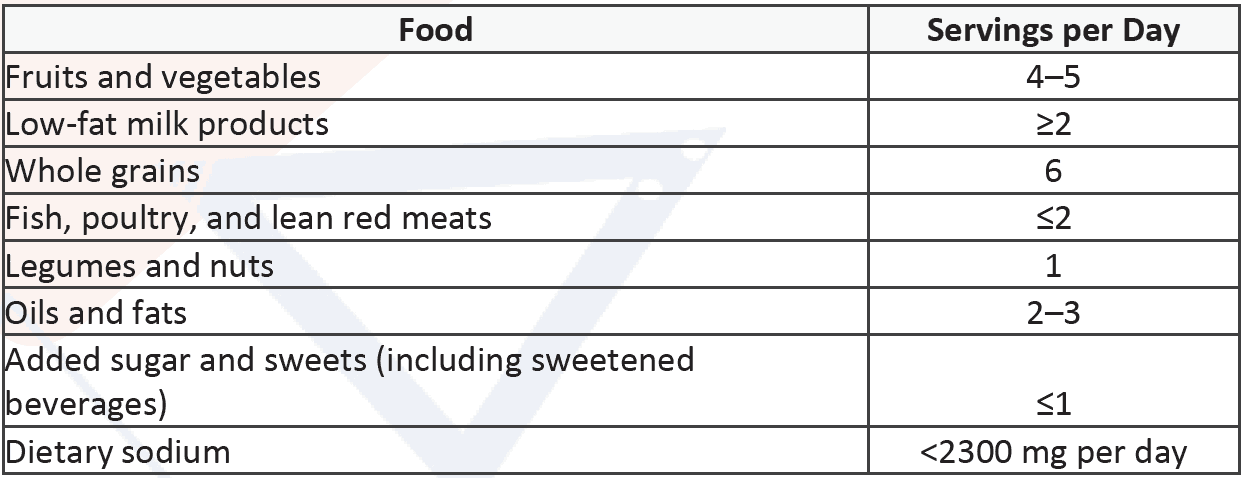
The Dietary Approaches to Stop Hypertension (DASH):
Table 11: DASH Diet Recommendations
Physical Activity & weight reduction
Advice on moderate to vigorous physical activity at least 3 to 5 days per week (30–60 minutes per session) to help reduce BP.
Stress Reduction to reduce 24-hour SBP (3–4 mmHg) and DPB (1 mmHg) in elevated BP.
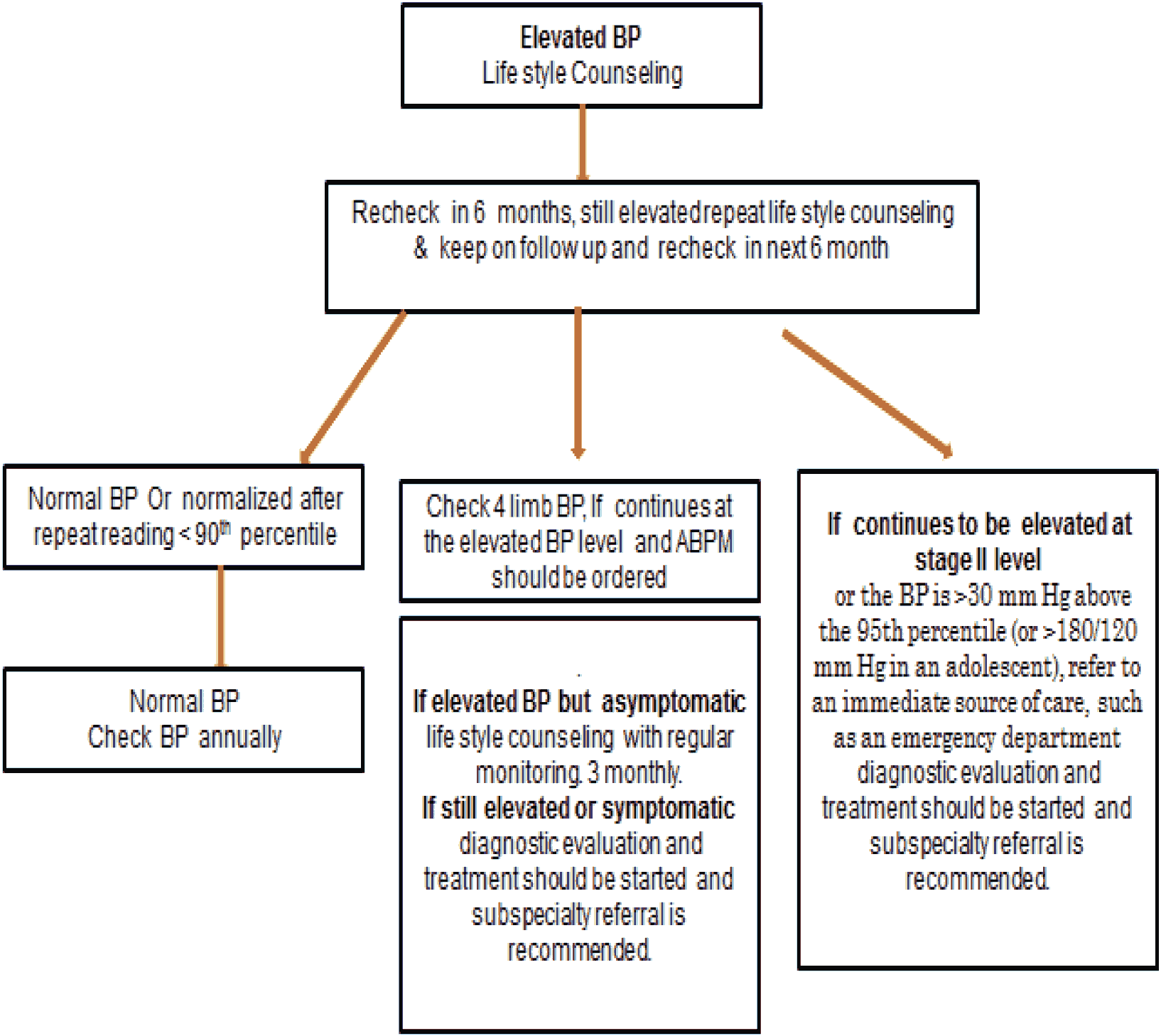
Figure 11: Algorithm of non-pharmacologic Interventions in Elevated BP
2. Pharmacologic Treatment
a. Choice of antihypertensive in children
- Treatment should be initiated with an ACE inhibitor/ ARB.
- Long-acting calcium channel blocker, or a thiazide diuretic
- Β-blockers are not recommended as initial treatment in children.
b. Treatment approach should be as follows:
Start with mono therapy with low dosage and increase up to mid-dosage range depending on response. Then if BP is not improved, add 2nd drug of different class but with complementary mechanism of action. In this approach, dose-dependent adverse effects of drugs can be avoided.
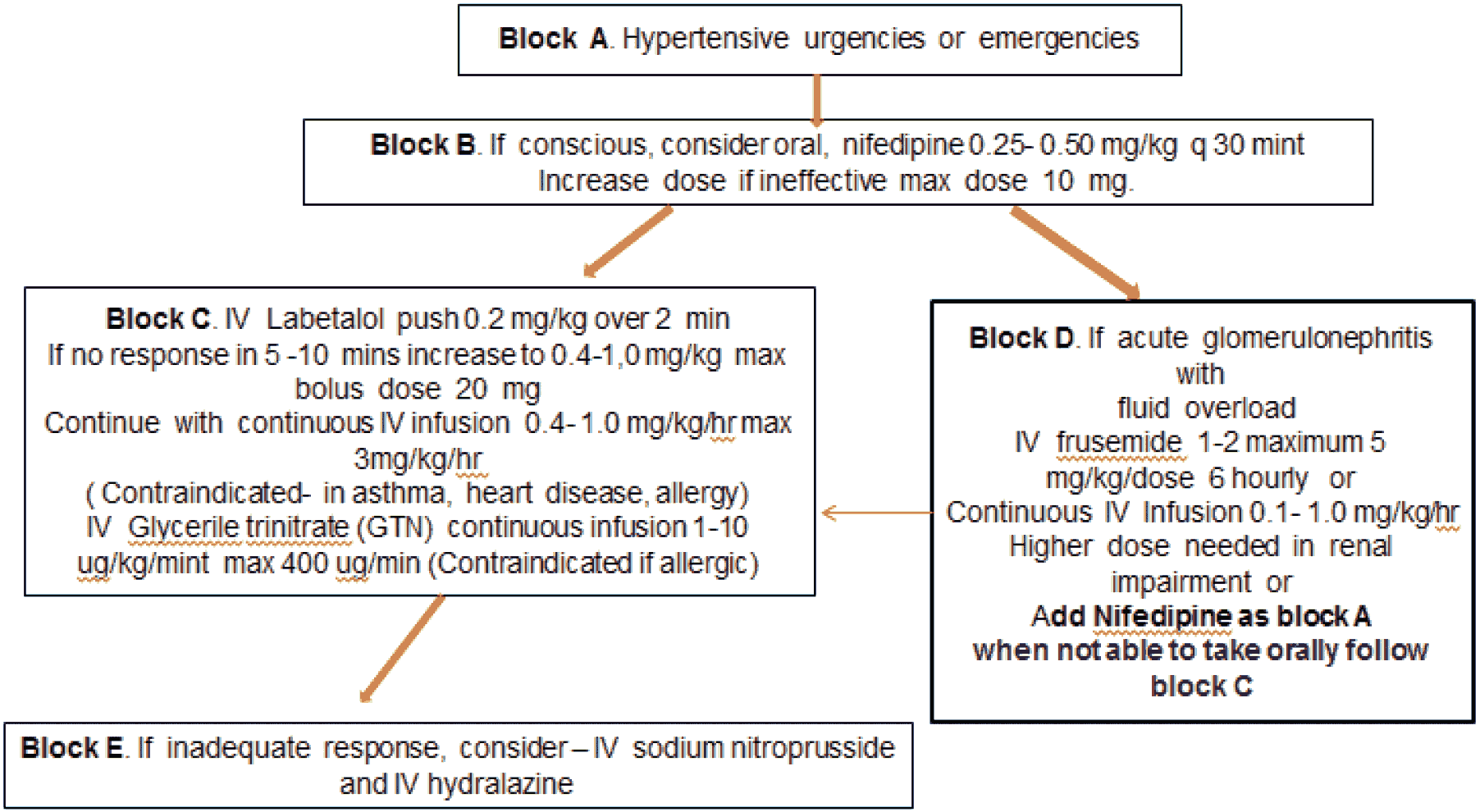
c. Treatment approach of severe HTN should be as follows:
Hypertensive emergency: symptomatic with complaints such as nausea, dyspnea, headaches and blurred vision. End organ damage such as cerebral infarction, cerebral hemorrhage, encephalopathy (altered mental status or seizures), pulmonary edema and kidney failure.
Hypertensive urgency: no end organ damage, no or minimal symptoms
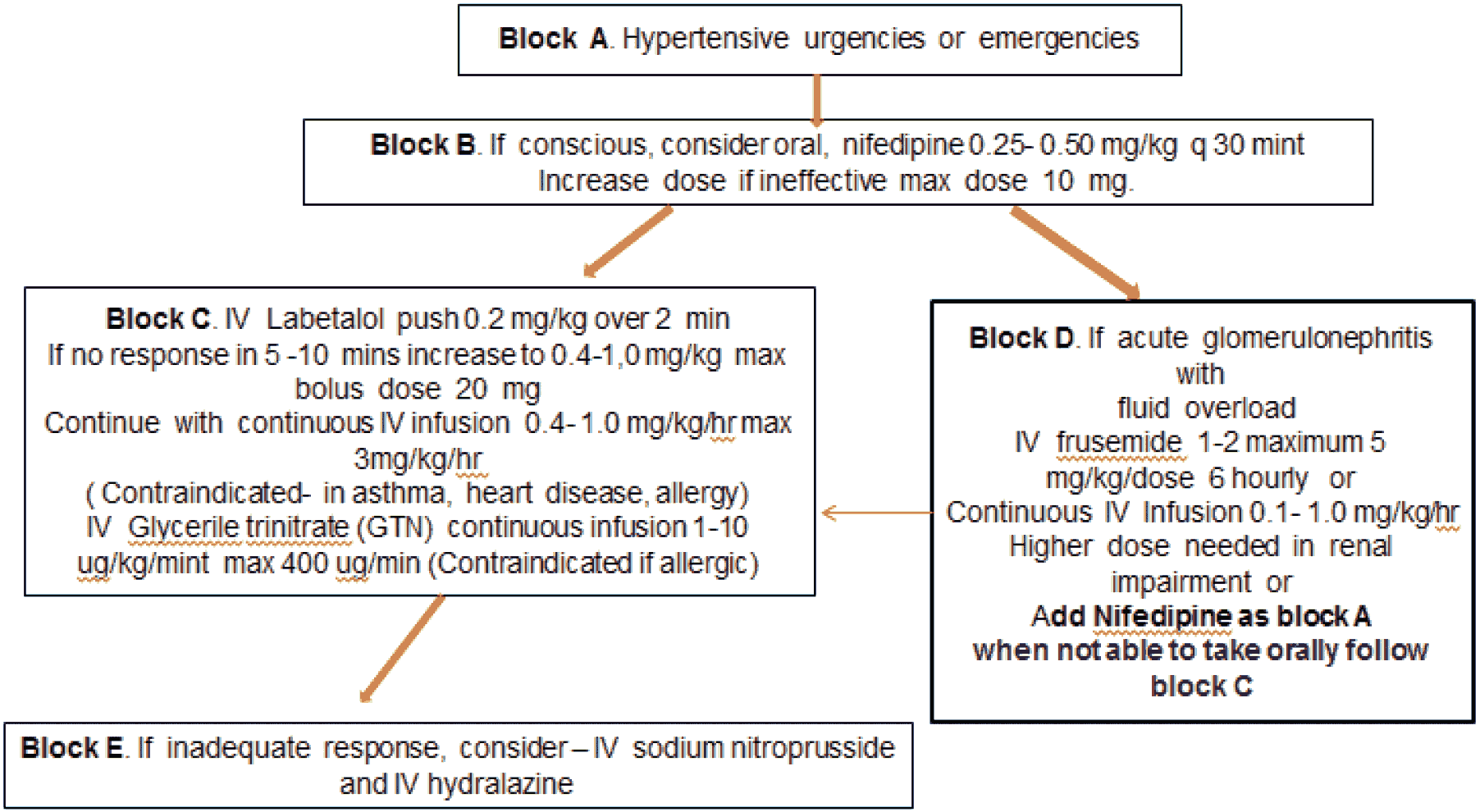
- Maintenance treatment with appropriate oral antihypertensive like ACE inhibitors and or Ca channel blockers. ACE inhibitors and ARBs are contraindicated in Acute Glomerulonephritis due to adverse effects of hyperkalemia and raised serum creatinine. Convulsion to be controlled simultaneously with per rectal diazepam 0.5mg/kg or injection Midazolam (0.2 mg/kg slowly mixed with distilled water).
d. Secondary Causes:
Renal and/or Reno vascular
Renal parenchymal disease and renal structural abnormalities account for 34% to 79% of secondary HTN. ACE inhibitors and ARBs are the choice of anti- hypertensive.
Cardiac, Including Aortic Coarctation
Coarctation of the aorta (CoA) is associated with HTN and right arm BP that is 20 mm Hg (or more) greater than the lower extremity BP. Relief of CoA is the mainstay of treatment.
Endocrine HTN
HTN resulting from hormonal excess accounts for a relatively small proportion of children with secondary HTN. Although rare (prevalence 0.05% to 6% in children). Treatment is according to cause.
3. Special situation:
Treatment of hypertension in Acute Post Streptococcal Glomerulonephritis (APSGN): See 2.C Block D.
Treatment of children and adolescent with chronic kidney disease (CKD) and hypertension
Children and adolescents with CKD should be evaluated for HTN at each medical encounter. Children or adolescents with both CKD and HTN should be treated to lower 24-hour MAP to <50th percentile by ambulatory blood pressure monitoring.
Treatment of children and adolescent with proteinuria and hypertension
Children and adolescents with CKD and HTN should be evaluated for proteinuria. Children and adolescents with CKD, HTN, and proteinuria should be treated with an ACE inhibitor or ARB.
Treatment of Patients with Diabetes
Children and adolescents with type 1 DM or type 2 DM should be evaluated for HTN at each medical encounter and treated if BP is ≥95th percentile or >130/80 mmHg in adolescents ≥13 years of age. Drug of choice ACEi (e.g., Ramipril) and or ARB (Losartan Potassium).
4. Hypertension with comorbidities
a. Dyslipidemia
Children with hypertension should be screened for dyslipidemia. Simvastatin for pediatric use with lifestyle advice, including weight loss and pharmacotherapy, as necessary.
b. Obstructive sleep apnea syndrome (OSAS)
Children with snoring, daytime sleepiness (in adolescents), or hyperactivity (in younger children) may have OSAS and consequent HTN. Symptomatic children with signs of OSAS (e.g., daytime fatigue, snoring, hyperactivity, etc.) should undergo evaluation for elevated BP. The use of ABPM is the recommended method for assessing the BP of children with suspected OSAS. In these children hypertension may not resolve even after treatment of OSAS with continuous positive airway pressure or adenotonsillectomy.
c. Hypertension in athletes
It is recommended that athletes with hypertension be promptly referred and evaluated by a qualified pediatric medical subspecialist within 1 week if they are asymptomatic or immediately if they are symptomatic. In stage 2 HTN children be restricted from high-static sports in the absence of end organ damage, including LVH or concomitant heart disease, until their BP is in the normal range after lifestyle modification and/or drug therapy.
Complications
Children who have high blood pressure are likely to continue to have high blood pressure as adults unless they begin treatment. A common complication associated with high blood pressure in children is sleep apnea, a condition in which a child may snore or have abnormal breathing when he or she sleeps. Children who have sleep-disordered breathing, such as sleep apnea, often have problems with high blood pressure - particularly children who are overweight. If, as often happens, a child’s high blood pressure persists into adulthood, the child could be at risk of stroke, heart attack, heart failure, kidney disease.