It depends on the level of BP, previously known as hypertensive or not, and whether on any medication. It is better to wait for 5-7 days in case of mild to moderate blood pressure rise (up to 180/110 mmHg) in previously unknown hypertensive patients. In case of known hypertensive or on treatment, the physician should continue the previous medication or add an anti-hypertensive drug. But one should be careful about precipitous fall of blood pressure; it should be reduced to target over 2-3 days. In the case of previously unknown hypertensive patients without any target organ damage, treatment should be started after 5-7 days. In case of target organ damage, it should be started immediately but slowly buildup to reduce BP gradually. Again, in the case of a thrombolysis candidate, blood pressure should be reduced below 185/110 mmHg and blood pressure should be maintained <180/105 for first 24-hour after the treatment. In patients for whom mechanical thrombectomy is planned and who have not received IV fibrinolytic therapy, it is reasonable to maintain BP ≤185/110 mmHg before the procedure. If there is severe hypertension (>220/120 mmHg), an immediate reduction of BP is necessary (10-20% reduction of the BP in first hour, up to 160/100 mm in 6 hours, Reduce to target in 2-3 days).
6.5 Hypertension Management in Stroke
exp date isn't null, but text field is
Stroke is the second most common cause of mortality and the most common cause of disability worldwide. The prevalence of stroke in different parts of the world is 4.7- 10.2/1000 and in Bangladesh is from 3-9 per 100021,22. Hypertension is the most common risk factor for a stroke of any type. In addition to the degree and duration of hypertension, both systolic and diastolic BP are equally responsible for a stroke. As stroke occurs commonly in the elderly, systolic BP is more related to stroke at admission, and 70-80% may have high BP immediately after the stroke. The incidence of stroke is 3 times higher in persons with stage 2 or stage 3 hypertension, and a reduction of systolic BP 10-12 mmHg and diastolic BP 5-6 mmHg is associated with a 38% reduction in stroke incidence.
The treatment of hypertension in acute stroke is controversial. About 10-20% of patients with acute stroke may have reactionary high BP for 5-7 days. Usually, mild to moderate reactionary blood pressure does not need treatment. A significant fall or increase in BP is associated with poor outcomes in acute stroke. High BP (220/110 mmHg) during acute stroke aggravates cerebral edema and reduces cerebral perfusion pressure, resulting in more ischemia. On the other hand, lower pressure (<100/60 mmHg) aggravates ischemic penumbra, so a judicious approach is necessary for treating hypertension in acute stroke.
The treating physician should consider the following fundamental issues in managing hypertension in acute stroke23-27.
- When to initiate anti-hypertensive drugs?
- Type of stroke
- The target blood pressure
- Presence of co-morbid diseases
- How to reduce blood pressure?
- Drug selection
- Whether a candidate for rt-PA or not
- Duration of treatment
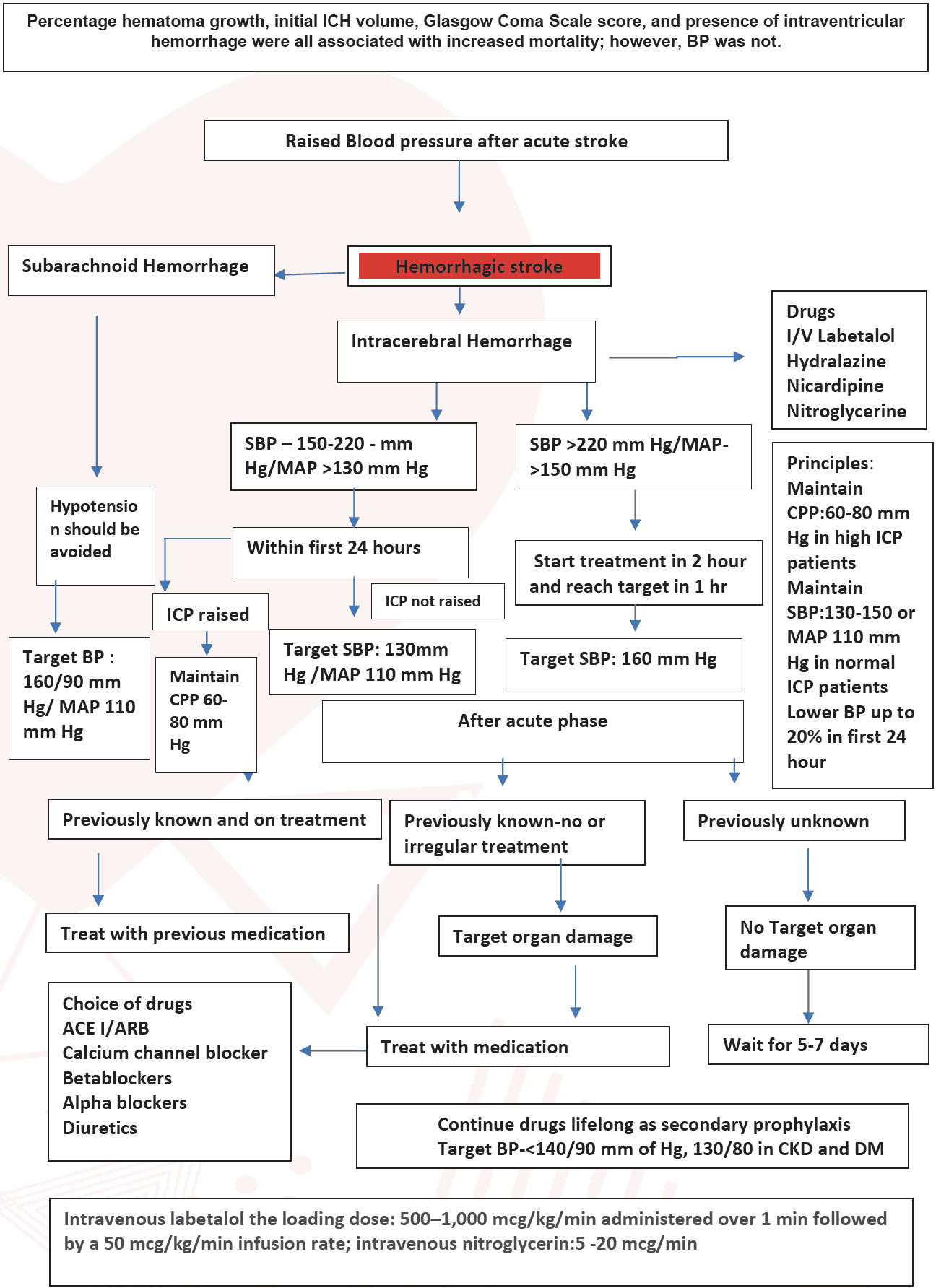
Stroke consists of ischemic (80-85%) and hemorrhagic (15-20%). Hemorrhagic stroke is again two types, intracerebral hemorrhage (ICH) (80-85%) and subarachnoid hemorrhage (SAH) (15-20%). The treatment strategy differs according to the type of stroke.
In hemorrhagic stroke:
If SBP >220 mm of Hg or mean BP >150, acute blood pressure reduction is necessary; starting treatment within 2 hours and reaching the target Blood pressure within 1 hour is recommended.
If the SBP is between 150-220 mm of Hg, it is reasonable to start antihypertensive as soon as possible and gradually titrate the BP to <130 mm of Hg. In case of raised ICP it is recommended to maintain cerebral perfusion pressure of 60-80 mm of Hg. For the secondary prevention target BP is <140/90 mm of Hg in general and <130/80 for CKD and diabetic patient.
In subarachnoid hemorrhage:
In subarachnoid hemorrhage, the risk of rebleeding is higher if the systolic blood pressure is>160 mm of Hg. Acute lowering of SBP to 140-160 mm of Hg is beneficial. But maintaining the cerebral perfusion pressure (CPP) at 60-80 mm of Hg is essential. Avoiding large degrees of blood pressure variability improves clinical outcomes in aneurysmal SAH.
In ischemic stroke:
The treatment of BP is generally the same as mentioned earlier. e.g., no immediate treatment in mild to moderate hypertension except in previously known hypertensive or if there is any target organ involvement. If there is severe hypertension, it needs immediate treatment by the agents mentioned above.
In ischemic stroke, Mean Arterial Pressure (MAP) is to be kept around 105- 110 mmHg, but if there is target organ involvement, MAP should be approximately 90-95 mmHg. In hemorrhagic stroke, the target BP is 5 mm more in SAH and 5 mm less in ICH than in ischemic stroke.
If there is any other co-morbid disease, e.g., renal failure, diabetes mellitus, cardiac failure, these should guide the drug selection. The target mean BP is around 100 mmHg.
- Anti-hypertensive treatment in people with acute ischaemic stroke is recommended only if there is a hypertensive emergency with one or more of the following serious concomitant medical issues:
- Hypertensive encephalopathy
- Hypertensive nephropathy
- Hypertensive cardiac failure/myocardial infarction
- Aortic dissection
It is a rule to reduce BP slowly in treating hypertension in acute stroke. The agents which reduce BP Slowly are preferred except in severe hypertension. No more than 20% reduction in any situation within 24 hours. Always oral agents are preferred.
It is crucial to select drugs judiciously. Many groups of anti-hypertensive agents are on the market, but all are not equally preferred for stroke. Few multicentric trials showed ARB or ACEI has an additional benefit in stroke. Among all the groups of drugs according to the priority of ARB, ACEI, Calcium Channel Blocker, Alpha Blocker, Beta Blocker, and Diuretics are used. The use of diuretics needs particular attention because sometimes the stroke patient may be dehydrated and have hyponatremia. The use of diuretics may aggravate the situation. For intravenous use IV labetalol, Nicardipine and Clevidipine are recommended drugs.
If the patient is a candidate for r-tPA, then there is necessary intervention because high BP >185/110 mm Hg is a contraindication for rt-PA in ischemic stroke. Blood pressure should be maintained <180/105 for the first 24-hour after the treatment. The approach is the same for ischemic stroke.
Blood pressure medication is to be continued for life because blood pressure is not a curable disease. It has to be kept under control by medication. There are some misconceptions about BP treatment among the general population as some people may have an idea that if drug treatment is started, then it will continue lifelong, so it is better not to start; some feel that with medication, if the BP is under control, the drug can be stopped. Somebody thinks it is better to take medicine when the symptoms appear, but all these are harmful. It is wise to start treatment and continue treatment because many severe complications of hypertension can be avoided if the BP is controlled.
Figure 9: Flow chart for management of ischaemic stroke with hypertension
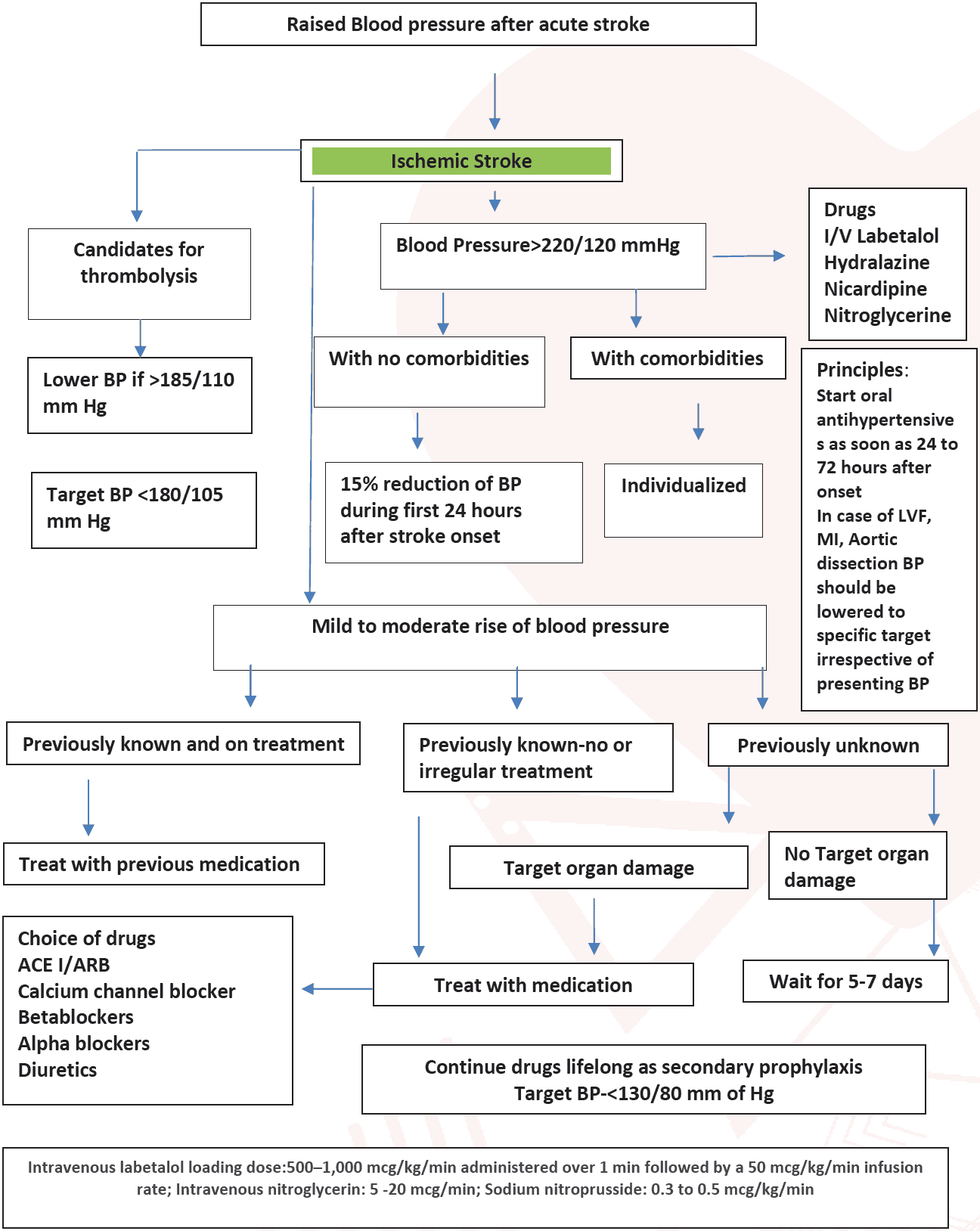
Whether a candidate for r-TPA or not: If the patient is a candidate for r-tPA, then intervention is necessary because high BP >185/110 mm Hg is a contraindication for rt-PA in ischemic stroke. The approach is the same for ischemic stroke.
