The approach to the treatment of hypertension in diabetes should be very much along the guidelines for treatment of hypertension in general. Nonetheless, a few important issues concerning nonpharmacological management and drug treatment need to be highlighted.
Non-pharmacological management
Dietary counseling should target optimal body weight and take into consideration glycaemic control and the management of concomitant dyslipidaemia. Moderate dietary sodium restriction is advisable. It enhances the effects of BP lowering drugs especially ACEIs and the ARBs. Further sodium restriction, with or without a diuretic, may be necessary in the presence of nephropathy or when the BP is difficult to control.
Pharmacological management
The use of certain classes of antihypertensive drugs may be disadvantageous to the diabetic patient by virtue of their modes of action or adverse effects. Diabetic control may be compromised, and various diabetic complications aggravated.
- Decreased insulin responsiveness with higher doses of diuretics
- masking of early symptoms of hypoglycaemia with beta-blockers and slowing of recovery from hypoglycaemia with non-selective beta-blockers
- Aggravation of symptoms of peripheral vascular disease with beta-blockers
- Dyslipidemia with most beta-blockers and diuretics
- Worsening of orthostatic hypotension with peripheral alpha blockers or centrally acting drugs.
ACEIs are drugs of choice based on extensive data attesting to their cardiovascular and renal protective effects in diabetic patients. In addition, they do not have adverse effects on lipid and carbohydrate metabolism. If an ACEI is not tolerated, an ARB should be considered. They have been shown to be of similar efficacy as ACEIs but better tolerated. There have been no reports of adverse effects on carbohydrate and lipid metabolism. Diuretics can be used as initial therapy or added on when mono therapy is inadequate. The lowest possible dose should be used to minimize adverse metabolic effects. Also, adverse metabolic effects with higher doses of diuretics have also been reportedly reduced when used in combination with an ACEI or an ARB.
CCBs do not have significant adverse metabolic effects or compromise diabetic control. Some studies suggest that non-dihydropyridine CCBs may be superior to dihydropyridine CCBs in reducing proteinuria in diabetic nephropathy. Beta-blockers may be used when ACEIs, ARBs or CCBs cannot be used or when there are concomitant compelling indications. However, they should be used with caution, especially in patients with type 1 diabetes. Peripheral alpha blockers do not have adverse effects on carbohydrate or lipid metabolism. Orthostatic hypotension due to autonomic neuropathy may be aggravated with their use.
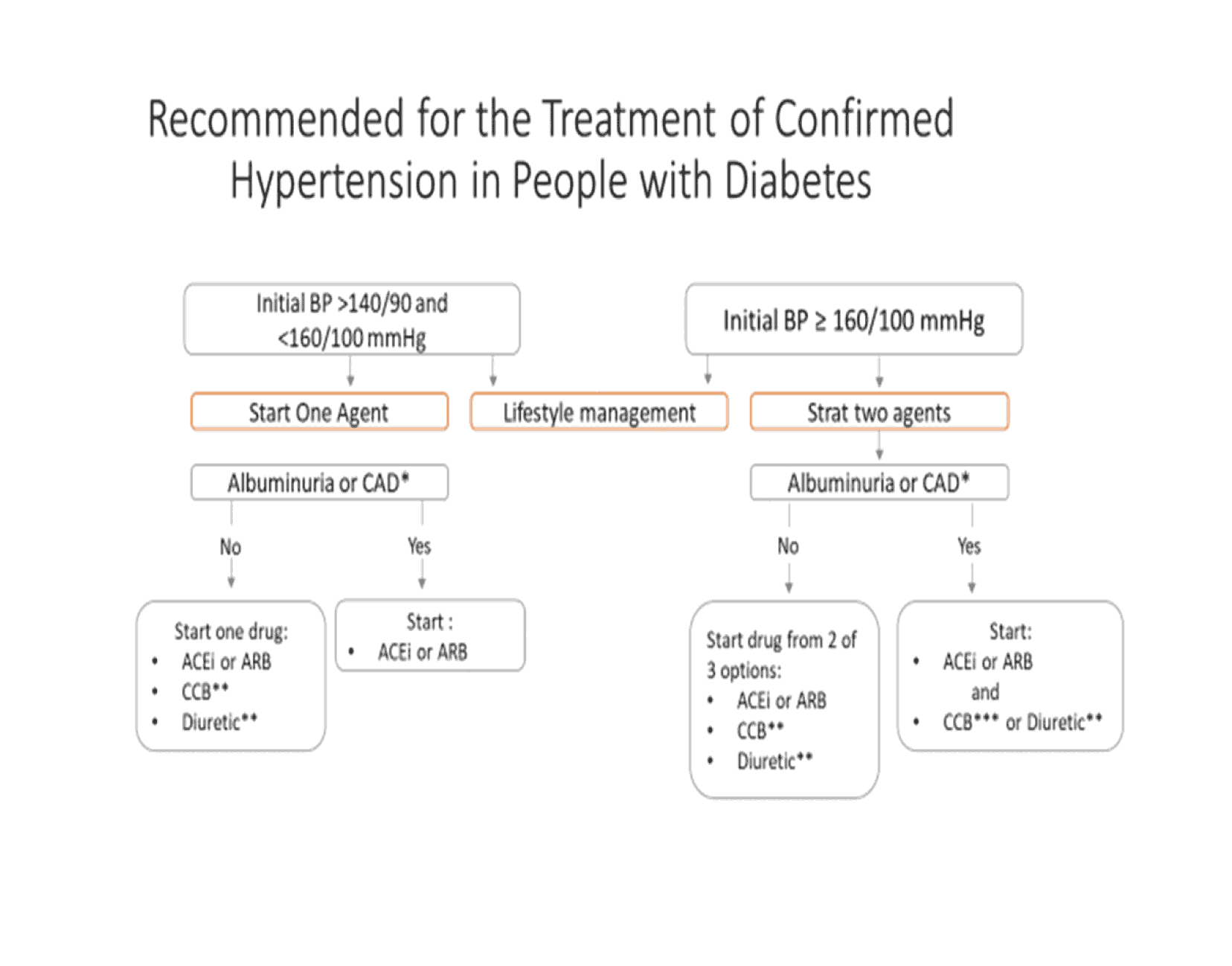
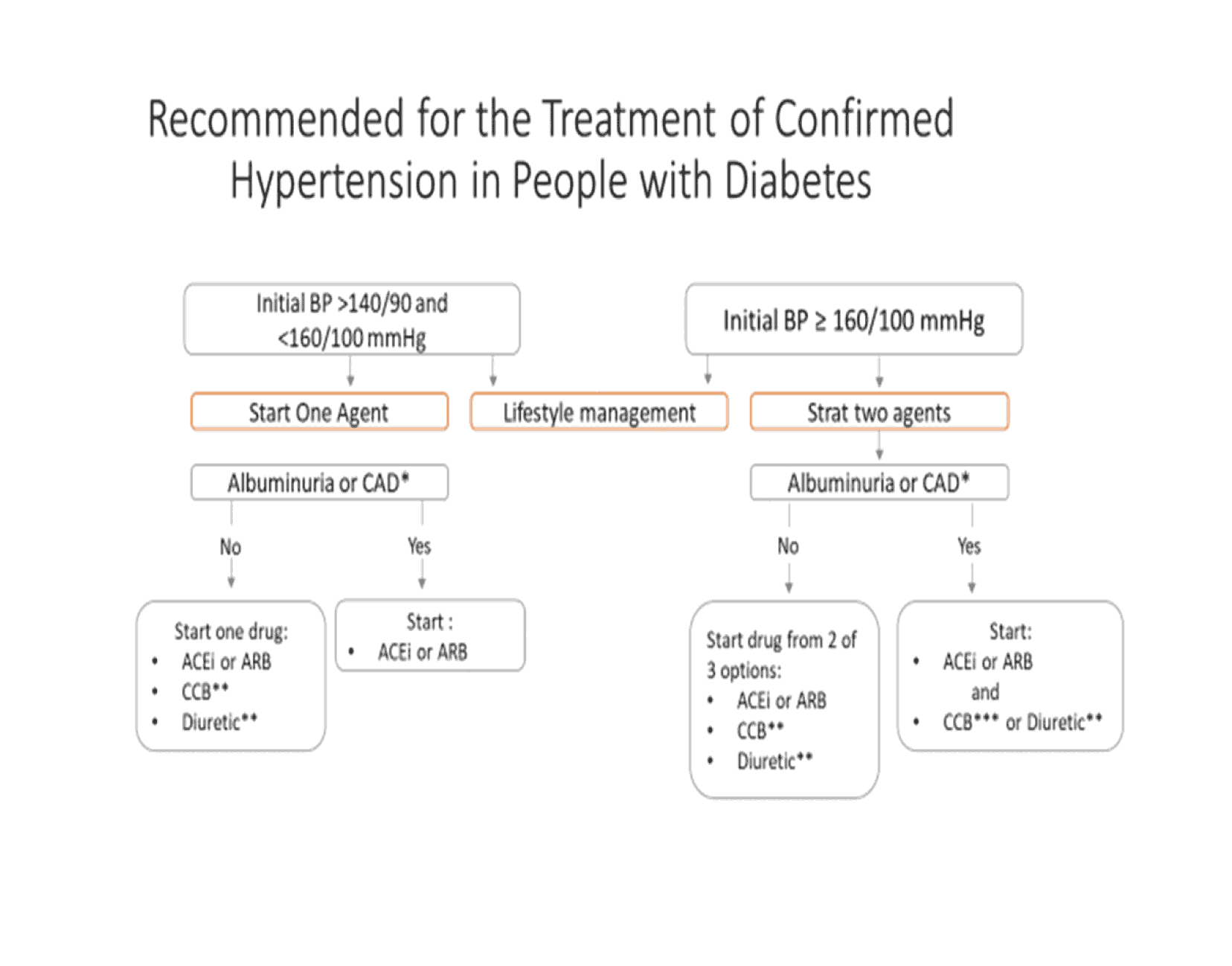
Figure 10: Schematic diagram for the management of high blood pressure in patients with diabetes mellitus