1.3 Strategies for control of Tuberculosis
exp date isn't null, but text field is
For effective control of tuberculosis and to prevent emergence of drug resistance, it is important to have a standard treatment policy for all patients in accordance with the internationally prescribed best-practices. Close co-operation of all healthcare providers at all levels is essential for successful implementation of the control programme. Similarly, the participation of community health workers, religious groups, political leaders and voluntary organizations is also essential for successful tuberculosis control. It is important that the community is informed of the nature and extent of the problem, as well as its prevention and cure. It must be stressed that the disease is curable and preventable and there is no reason for discrimination or stigma. Another key element in controlling tuberculosis is to ensure that patients are supported to take their medicines regularly till the successful completion of treatment. Non-adherence to prescribed treatment could lead to unfavourable outcomes, continued transmission and even drug resistance. All of these could potentially result in major setbacks faced by national tuberculosis programmes.
After having successfully implemented the DOTS strategy in Bangladesh, the country embarked on the other components of the WHO recommended Stop TB Strategy6 wherein the focus is on ensuring high quality DOTS, better outreach so that more number of patients have access to quality TB care, management of multi-drug resistant TB (MDR-TB) and TB-HIV co-infection, strengthening of health systems, involving all healthcare providers in the public sector, private sector and Non-Governmental Organizations (NGOs), strengthening the advocacy campaign, promoting Medical College involvement and research. The country has now endorsed and adapted the WHO End-TB strategy.
Pillars and Component
- Integrated patient centred care and prevention
- Early diagnosis of tuberculosis including universal drug-susceptibility testing and systematic screening of contacts and high-risk groups
- Treatment of all people with tuberculosis including drug-resistant tuberculosis; and patient support
- Collaborative tuberculosis/HIV activities; and management of comorbidities
- Preventive treatment of persons at high risk; and vaccination against tuberculosis
- Bold policies and supportive systems
- Political commitment with adequate resources for tuberculosis care and prevention
- Engagement of communities, civil society organizations, and public and private care providers
- Universal health coverage policy, and regulatory frameworks for case notification, vital registration, quality and rational use of medicines, and infection control
- Social protection, poverty alleviation and actions on other determinants of tuberculosis
- Intensified research and innovation
- Discovery, development and rapid uptake of new tools, interventions and strategies
- Research to optimize implementation and impact, and promote innovations
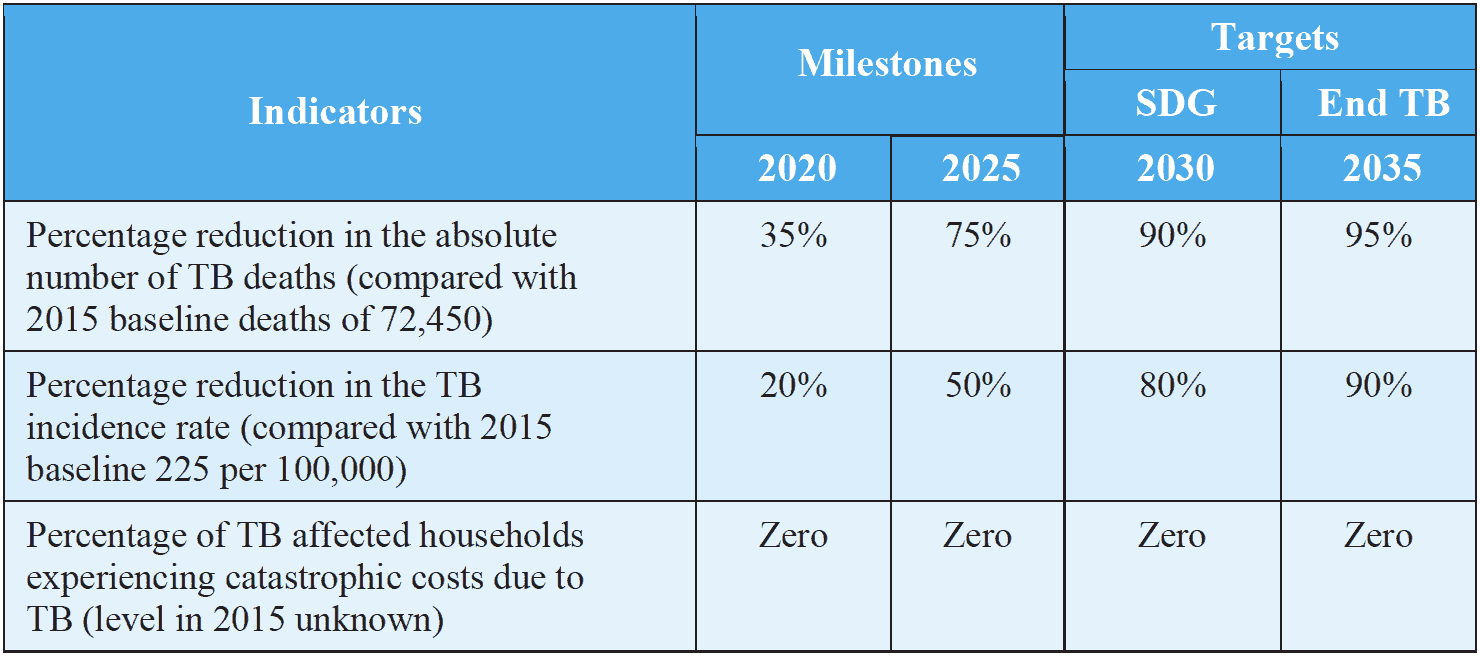
Targets related to End TB Strategy and SDG along with milestones are shown below:
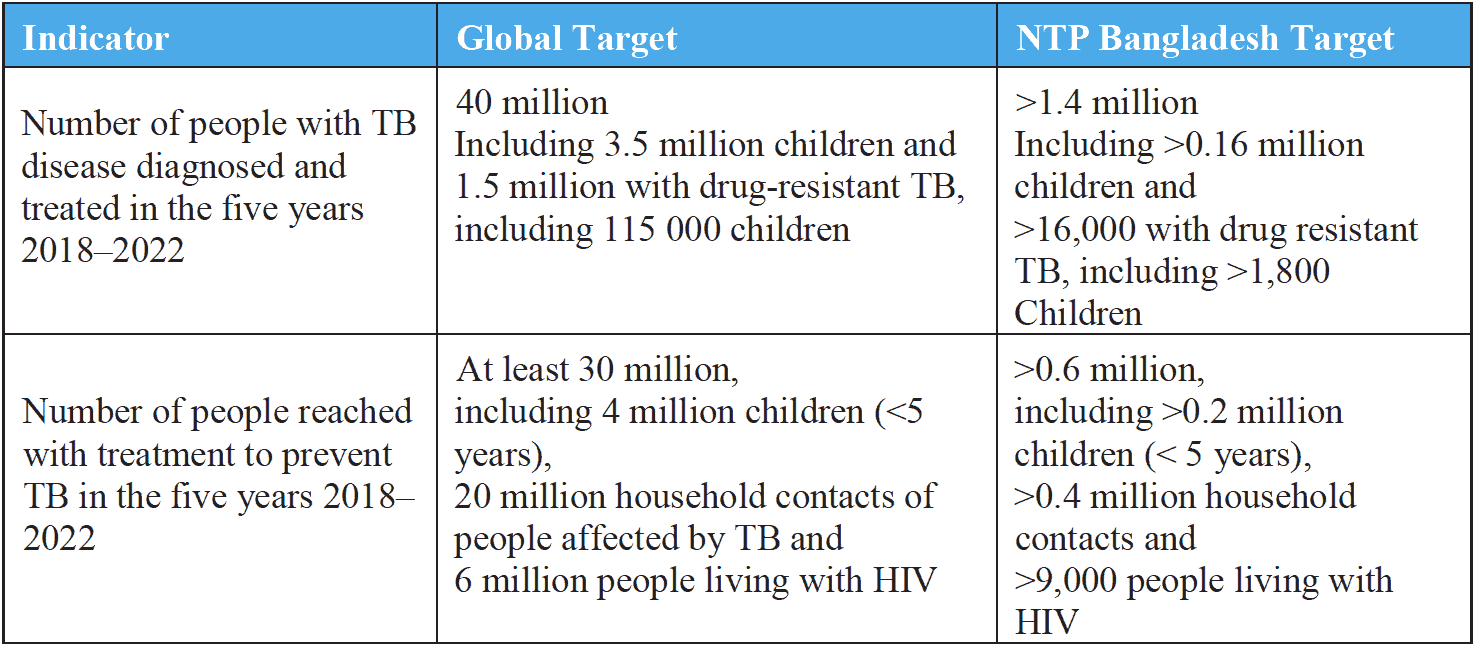
The first UN General Assembly high-level meeting on TB was held in New York on 26 September 2018, titled United to End TB: An Urgent Global Response to a Global Epidemic. The main outcome of the meeting was a political declaration7. This reaffirmed the commitment of Member States to the SDGs and the End TB Strategy, and to the actions required to accelerate progress that were defined in the Moscow Declaration. The NTP Bangladesh is fully committed to reaching the global targets defined during the UN high-level meeting and country-specific targets have been defined in line with the global goals.
6 The End TB Strategy; Global strategy and targets for tuberculosis prevention, care and control after 2015; WHO, Geneva, 2015
7 United Nations General Assembly. Resolution 73/3: Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. United Nations; 2018
