14.2 Nutritional assessment
exp date isn't null, but text field is
Nutritional assessment is a prerequisite for provision of appropriate nutritional support in patients with TB, and on follow-up of the patient. Nutritional assessment may vary according to the population groups, e.g., adult patients (above 18 years), children and adolescents (6–18 years), children under 5 years of age, and pregnant mothers.
Nutritional assessment will include the following:
- Clinical assessment: This includes a nutrition-oriented history and a nutrition-oriented examination
- Anthropometric assessment
- Dietary assessment and laboratory assessment wherever feasible and appropriate.
Assessment at diagnosis
It is important to identify undernutrition at the onset of diagnosis and establish the baseline of nutritional indicators to monitor the response to treatment in patients with TB. It is also important to identify children and adults who may be severely undernourished, with or without other complications and who may require initial treatment in a hospital.
Assessment at follow up
In patients who continue to be moderate- severely undernourished during follow-up, further risk factor and dietary assessment will be necessary, as follows:
- Poor TB treatment adherence and/or response, resistance to TB drugs
- Clinical assessment for other non-dietary causes of malnutrition, including identification of important co-morbidities such as diabetes, HIV, alcohol abuse.
- Biochemical assessment whenever possible
- Dietary assessment, including assessment of food security.
Weight loss or failure to regain or maintain a healthy weight, at any stage of disease should trigger further assessment and appropriate interventions. Nutritional status of patients with MDR-TB is particularly important as treatment outcomes in this group of patients are sub-optimal and poor nutritional status has been associated with greater frequency of side-effects, delayed time to sputum conversion and mortality.
A. Clinical assessment
Nutrition-oriented examination in patients with active TB
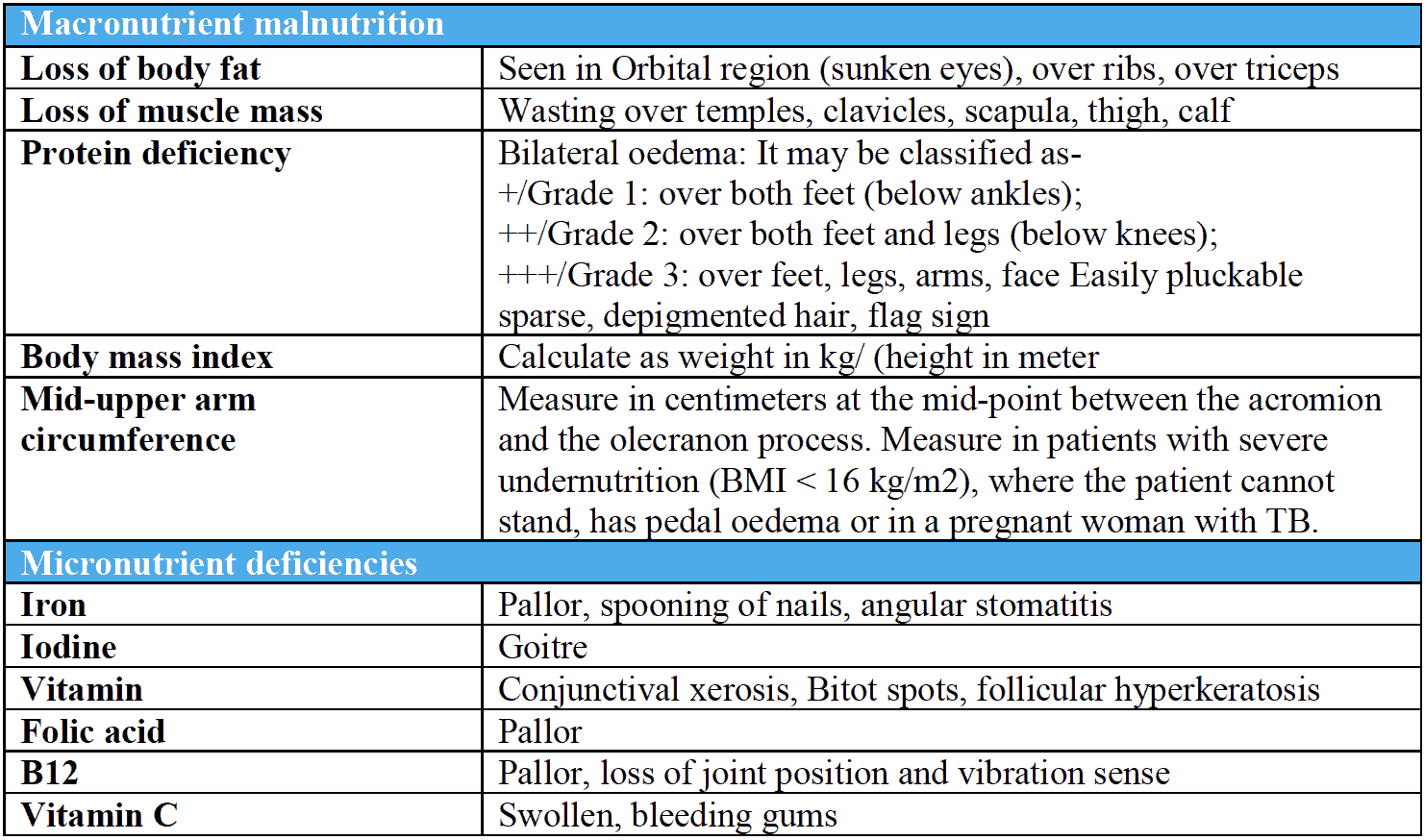
B. Anthropometric assessment
Height and weight: This is a measure of weight adjusted for height, which is calculated by dividing the weight in kg by the square of height in metres.
BMI= ��������ℎ�� ���� ����/ (��������ℎ�� ���� ��)2
BMI is useful as a measure of the fat and muscle mass of the body. It is also useful as an indicator of risk of morbidity and mortality, which increase linearly in subjects with both BMI higher and lower than normal. At higher BMI, the risk of CVD deaths increases, while at lower BMI subjects are at greater risk of dying due to respiratory causes including TB.
Classification of nutritional status and associated risk using BMI as criteria
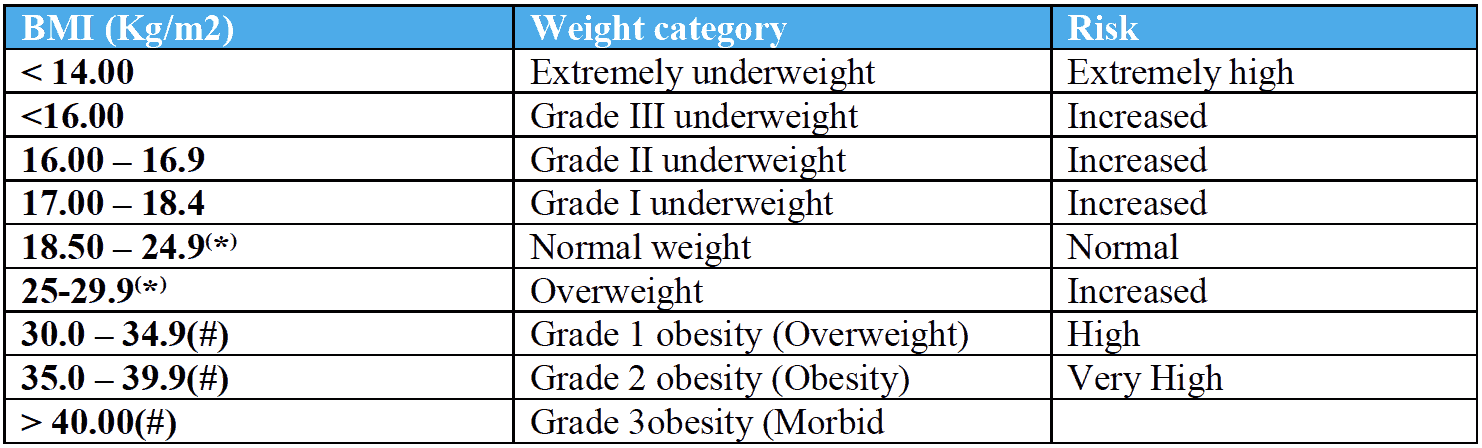
*A WHO expert consultation in 2004 proposed different cut-offs for overweight and obesity in Asians on the basis of available data which suggests that Asians have a higher percentage of body fat than White people of same age, sex and BMI. The consultation identified potential action points: Underweight BMI less than 18.5; Normal- BMI 18.5-22.9;
Overweight- BMI 23.0-26.9; Obesity-BMI> 27.0 (64).
# Situation not likely to be common in case of TB patients.
Mid upper arm circumference (MUAC)
MUAC is the circumference of the left upper arm -measured midway between the tip of the shoulder (acromion) and elbow (olecranon). It is an indicator of nutritional status (including fat and protein stores), and like the BMI is also independent of height. It can be measured in pregnant women and those who are unable to stand.
MUAC <23 cm in Men and < 22 cm in women correlates with a BMI of < 18.5 kg/m2 and is suggestive of undernutrition. MUAC reflects of the effect of acute undernutrition more than BMI, and has been seen to an independent predictor of mortality in both HIV positive and HIV negative individuals. Patients with a MUAC less than 19 cm had 5 times the mortality rate of those with a MUAC > 24 cm. There are no standard MUAC cut-offs for different grades of adult undernutrition. In WHO Integrated management of Adolescent and Adult illness, a cut-off of MUAC < 16 cm was used to define severe undernutrition. However, a cut off of less than 16 cm would correspond to a situation of virtually no peripheral energy stores, and excess mortality has been seen at levels of MUAC which are higher than this cut-off in patients with active TB.
Propose criteria for initiation of nutritional support in an inpatient setting for adults (>18 years):
Suggested cut-offs for MUAC for moderate – severe undernutrition in adults
MUAC < 19 cm: Severe undernutrition
MUAC 19–22 cm: Moderate acute malnutrition
C. Biochemical and laboratory evaluation
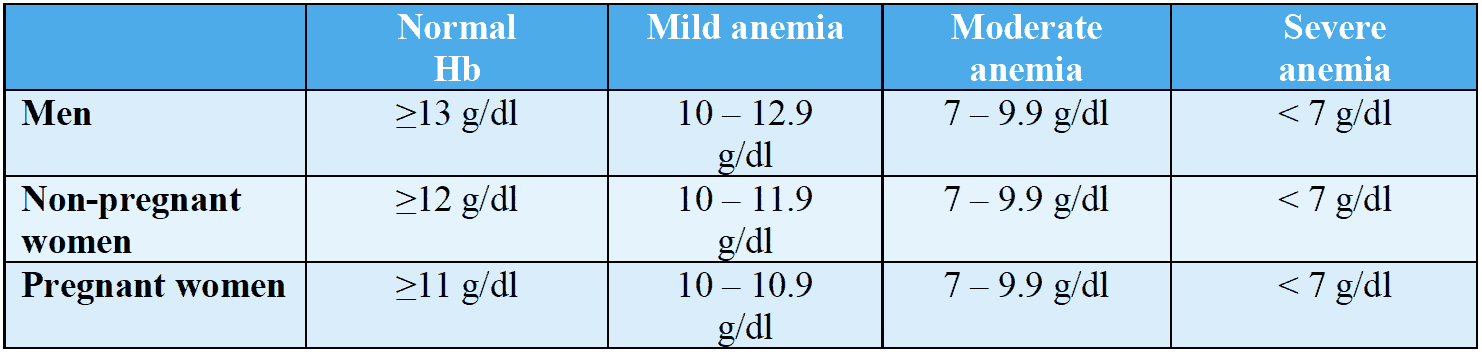
Hemoglobin:
Anemia due to deficiency of micronutrients like iron and folates is very common in patients with TB and can contribute to poor performance status in patients with TB.
Criteria to classify anemia in males and females (WHO)
Serum albumin
Is affected by malnutrition but is also affected by inflammation. The normal range is 3.5 to 5.5 g/dL. In patients with TB, hypoalbuminemia (e.g., serum albumin less than 2.7 g/dl) has been associated with increased risk of death, while a higher albumin was inversely related to treatment failure in patients with extensively drug resistant TB
Serum electrolytes
Measurement of serum potassium and magnesium is desirable, if patient has severe undernutrition and has been admitted for inpatient management. This is because patients with severe undernutrition are deficient in these, and low levels of potassium and magnesium are risk factors for re-feeding syndrome
