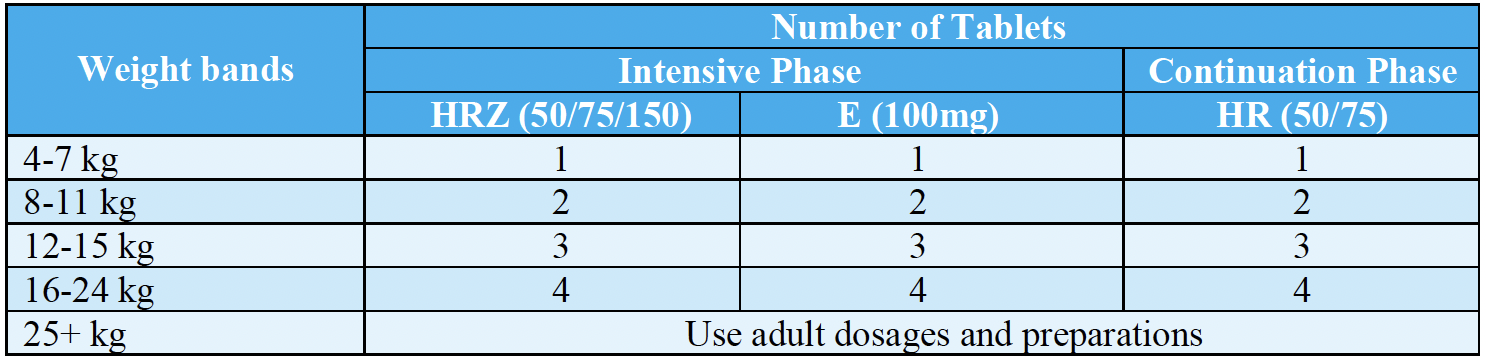
Anti-TB treatment is divided into two phases: an intensive phase and a continuation phase. The purpose of the intensive phase is to rapidly eliminate the majority of organisms and to prevent the emergence of drug resistance. The purpose of the continuation phase is to eradicate the dormant organisms.
TB drugs for the treatment of TB in children come in Fixed Dose Combinations (FDC) and dosed according to standardized weight bands. Depending on their weight, children can be treated using the pediatric FDCs or the adult FDCs. Older children falling into higher weight ranges will receive adult FDCs.
All children must be treated using child-friendly (dispersible and flavoured) FDC. The new fixed-dose combination of HRZ (50 mg / 75 mg / 150 mg) and HR (50 mg / 75 mg).
Ethambutol is included for the treatment of TB in children and comes as a separate tablet (to monitor ophthalmic ADRs) with the paediatric formulation (100 mg).
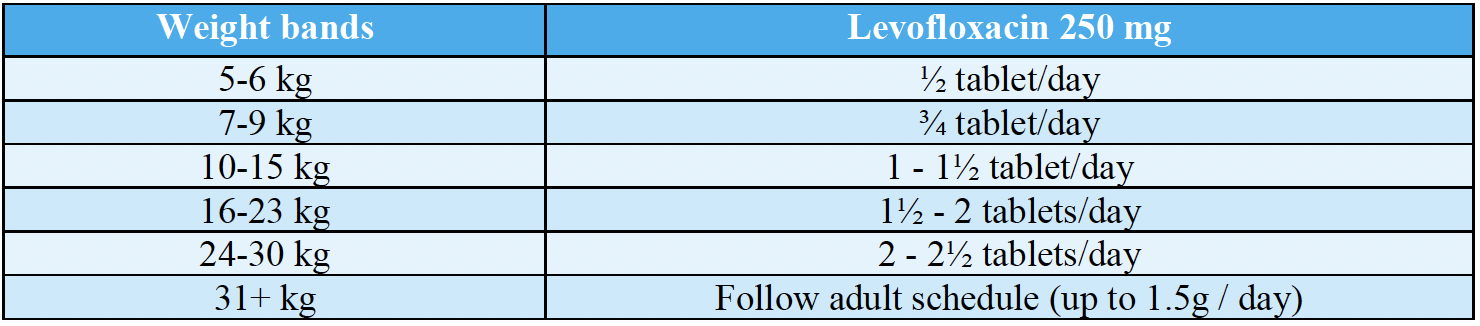
Weight band for INH mono resistant TB (Hr-TB)
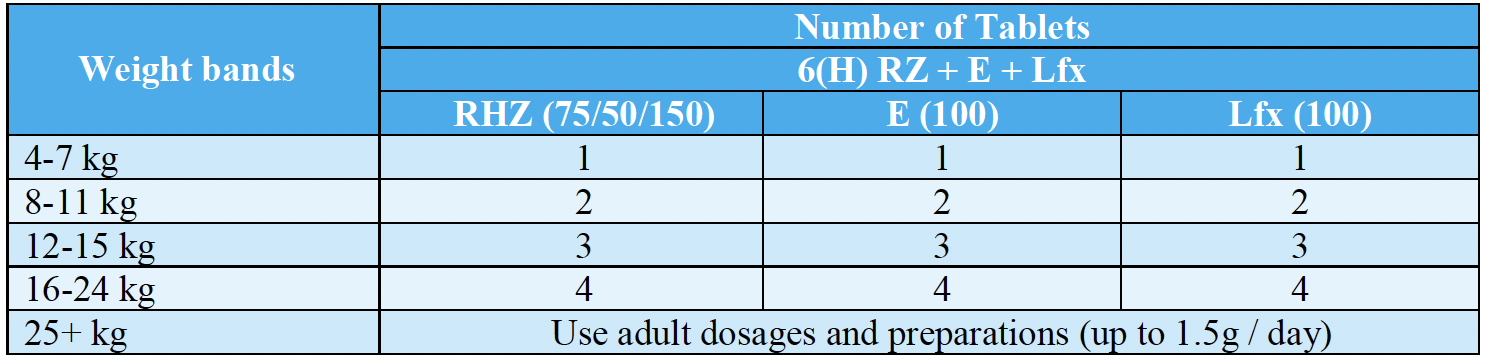
If levofloxacin 100mg dispersible tablet is not available, the 250mg tablet can be used with 6(H) RZ+E in children aged 0-14 years, based on a slightly different weight band from the one above: